Certain Seasonings And Condiments
The following seasonings and condiments are safe for those following gluten-free diets:
- apple cider vinegar
- fresh herbs like basil, rosemary, and cilantro
- pesto
Most sources of healthy fat, such as the following, are gluten-free.
- full fat yogurt
- unsweetened coconut, as well as coconut oil
Summary
Foods that are safe to eat if you have a gluten intolerance include nuts, seeds, vegetables, fruits, fish, poultry, dairy products, gluten-free grains, and legumes.
What Are The Practical Aspects Of Living With Celiac Disease
A gluten-free diet will be a big change in your life . You have to rethink your eating habits, including what you buy for lunch, what you eat at parties, or what you snack on. When you go grocery shopping, be sure to read the ingredient labels carefully to avoid accidental gluten ingestion. If after reading labels you are not sure about gluten content, it is not safe for you.
A dietitian, a healthcare professional who specializes in food and nutrition, can help you with the gluten-free diet. There are also support groups that can help patients who have just been diagnosed with celiac disease.
How Is Gluten Intolerance Diagnosed
Your healthcare provider carefully reviews your symptoms and medical history. If they suspect you have a gluten intolerance, these are the next steps to confirm the diagnosis:
- Step 1: You eat a diet containing gluten for about six weeks. During this time, your healthcare provider performs blood tests and skin tests to rule out a wheat allergy or celiac disease. There isn’t a gluten intolerance test.
- Step 2: If you don’t have a wheat allergy or celiac disease, your healthcare provider will ask you to exclude gluten from your diet for at least six weeks. Keep a thorough record of your symptoms during this time, noting which symptoms improve.
- Step 3: If your symptoms do improve while you’re on a gluten-free diet, you gradually reintroduce gluten back into your diet. If symptoms return, you likely have a gluten intolerance.
Several Processed Foods And Other Items
Many processed foods and other popular items may also harbor gluten. These include:
- meat substitutes, such as veggie burgers and hot dogs
- prepared lunch meats
- canned soups and soup mixes
- puddings and instant dessert mixes
- certain ice creams
- french fries and other fried foods
- flavored tofu
Summary
Foods that contain gluten include breads, pastas, crackers, baked goods, many grains, and several beverages and processed items.
Though it may seem as if most foods are off-limits when you’re intolerant to gluten, many delicious and healthy foods are naturally gluten-free. Plus, quality gluten-free breads, pastas, and crackers are available in most grocery stores.
If you’re gluten intolerant, you can enjoy the following foods.
Diagnosing And Treating Wheat Allergy
To diagnose a wheat allergy, doctors usually use what’s called “skin prick” tests, in which your physician will prick your skin with tiny needles containing a small amount of wheat protein. If you develop a red bump on your skin where it was pricked within 15 minutes, you’re likely allergic to wheat. Your doctor may also order IgE or other blood tests to help diagnose a wheat allergy, or possibly ask you to keep a detailed list of the foods you eat, along with a record of your symptoms, to aid in diagnosis.??
Treatment of wheat allergy usually involves staying away from foods that include wheat. However, your doctor may prescribe antihistamines to help you manage symptoms when you’ve been exposed. In addition, if your allergy is severe, or if it can result in potentially life-threatening symptoms, your doctor may recommend that you carry in the form of an Epi-Pen to treat yourself immediately upon exposure.
Wheat is considered one of the top eight food allergens in the U.S., so companies must, therefore, companies disclose when they include a wheat-containing ingredient in a food product.?? Since many gluten-free foods are also wheat-free, people with wheat allergy have benefited from the explosion in gluten-free food products in recent years.
Learn more:
What Are The Specific Challenges To Children And Teens With Non
While non-celiac gluten sensitivity appears to be less common in children and teens, the negative impact of a gluten-free diet is far reaching in a child’s life. Because of the varied symptoms and lack of clear diagnostic criteria, non-celiac gluten sensitivity can be missed in children.
- The symptoms more commonly seen in children tend to be neurological and may be attributed to the child’s behavior rather than an underlying physical cause. Symptoms can include brain fog, attention issues, headaches, and dizziness.
- Children with non-celiac gluten sensitivity can also experience joint and muscle pain, which may be dismissed as growing pains.
- Symptoms may have a substantial impact on school attendance and performance and the ability to socialize. Once diagnosed, the gluten-free diet adds another layer of complication. Many schools provide meals for children, but a safe gluten-free meal may not always be an option. This may also be true for summer camps, sports activities, and school functions and trips.
- There are also the social limitations of the diet. Children may feel isolated or may be bullied because they have different dietary needs. This might lead older children and teenagers to be less strict with their gluten-free diet from time to time in order to feel that they fit in better with their peers.
Breach Of Intestinal Barrier
Loss of integrity of the plays a key role in IBD. Dysfunction of the as a result of abnormal signaling through immune receptors called —which activates an immune response to molecules that are broadly shared by multiple pathogens—contributes to acute and chronic inflammatory processes in IBD colitis and associated cancer. Changes in the composition of the are an important environmental factor in the development of IBD. Detrimental changes in the intestinal microbiota induce an inappropriate that results in damage to the intestinal epithelium. Breaches in this critical barrier allow further infiltration of microbiota that, in turn, elicit further immune responses. IBD is a multifactorial disease that is nonetheless driven in part by an exaggerated immune response to gut microbiota that causes defects in epithelial barrier function.
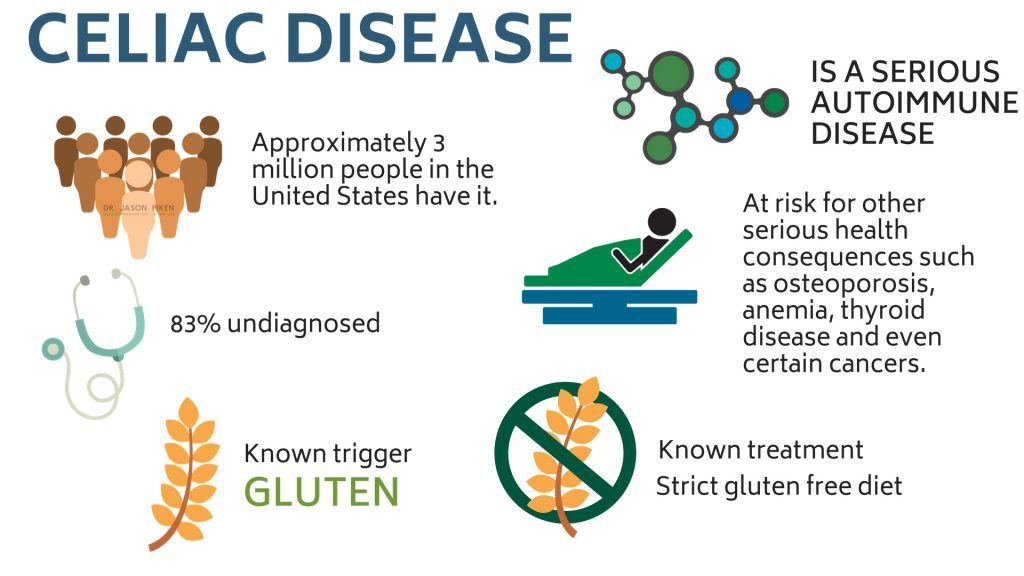
What Is Celiac Disease
According to the Celiac Disease Center at the University of Chicago, celiac disease affects roughly 1 in 133 people in the United States. An inherited autoimmune disorder, this condition affects the digestive process of the small intestine. When a person who has this disease consumes food that contains gluten, the immune system launches an attack against the gluten, mistakenly damaging healthy cells lining the small intestine in the process.
Over time, celiac disease-related autoimmune activity inhibits the small intestine’s ability to absorb nutrients from food which can lead to a wide variety of symptoms including chronic fatigue, brain fog, bone or joint pain, tingling in the hands or feet, and even depression or anxiety. As long as a person with celiac disease continues to consume gluten, damage can and will be done to the digestive system – a lifelong gluten free diet is the only known effective treatment for this condition.
The Blood Tests And Biopsy Used To Test For Cd Require A Patient To Be Eating Gluten To Obtain Accurate Results
If a patient is started on a gluten-free diet without evaluating celiac disease, it becomes challenging to appropriately diagnose celiac disease. Patients who experience clinical improvement on a gluten-free diet will rarely restart a gluten-containing diet to get an appropriate diagnosis. They finally feel well, and returning to being sick is just not an option. The importance of testing cannot be overemphasized. Consider these factors:
CD is lifelong,
We don’t know about GS. It is wrong to subject someone to a lifelong, strict gluten-free diet if they don’t need it. The social and psychological implications can be vast.
CD requires a strict gluten-free diet.
A gluten-free diet may not treat those with GS. They may require a low FODMAP diet. This difference in utilizing the proper diet can be life-changing to some patients.
CD is genetic
CD has long-term risks and complications.
These parameters may be different for GS. We simply don’t know yet. Appropriate diagnosis is necessary for and those with gluten sensitivity.
Insurance reimbursement can be more challenging without a diagnosis.
You and your patients are more likely to get insurance reimbursement for a diagnosis of CD that would otherwise be missed if never tested for.
Accommodations
To obtain ADA accommodations, students need documentation stating they have a diagnosis of CD or food allergies. At this time, GS does not appear to be covered under the ADA.
What Are The Causes Of Celiac Disease
Normally, the body’s immune system is designed to protect it from foreign invaders. When people with celiac disease eat foods that contain gluten, their immune systems attack the lining of the intestine. This causes inflammation in the intestines and damages the villi, the hair-like structures on the lining of the small intestine. Nutrients from food are absorbed by the villi. If the villi are damaged, the person cannot absorb nutrients and ends up malnourished, no matter how much he or she eats.
Diarrhea Constipation And Smelly Feces
Individuals with celiac disease experience inflammation in the small intestine after eating gluten.
This damages the gut lining and leads to poor nutrient absorption, resulting in significant digestive discomfort and frequent diarrhea or constipation (
).
That suggests that gluten exposure on its own may induce feelings of depression, irrespective to digestive symptoms.
Foods To Avoid With A Gluten Intolerance
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Many people avoid gluten, a group of proteins found in grains like wheat, barley, and rye, due to personal preference or a medical condition .
Celiac disease, wheat allergy, and non-celiac gluten sensitivity all involve an adverse reaction to gluten and are treated with a gluten-free diet. These conditions are considered forms of gluten intolerance .
While both celiac disease and NCGS may lead to intestinal damage and cause symptoms like diarrhea, gas, and bloating, celiac is an autoimmune condition linked to other serious health effects, such as anemia, stunted growth, and neurological effects .
Wheat allergy refers to an allergic reaction to wheat proteins, the symptoms of which may be life threatening. This condition is treated with a wheat-free diet, not necessarily a gluten-free diet .
Although people with wheat allergies must avoid wheat, most are able to eat other grains, including gluten-containing ones like barley and rye.
Meanwhile, people with celiac disease and NCGS must avoid all gluten-containing foods to control symptoms. Notably, many healthy foods are naturally gluten-free, and quite a few companies make scrumptious gluten-free products.
Here are 8 foods to avoid if you have a gluten intolerance, as well as 7 you can safely eat.
Causes And Risk Factors

Celiac disease is an autoimmune disorder. When a person who has it eats gluten, their immune system attacks and damages their small intestine.
Over time, finger-like projections in the intestine that absorb nutrients, called villi, get damaged, limiting the overall absorption. This can lead to a number of health issues.
Celiac disease can develop in anyone. It is more common in white people and in females.
Also, it runs in families. A person with a parent or sibling who has celiac disease has a 1 in 10 chance of developing it, too.
Celiac disease is more common in people with other conditions, including:
Are Gluten Intolerance And Celiac Disease The Same Thing
Gluten intolerance and celiac disease are different. People with celiac disease have an autoimmune response to gluten. This means their bodies try to fight against gluten as if it were a virus. This reaction causes inflammation and damage to their digestive tracts. Celiac disease is the result of an abnormal gene. People with celiac disease also have high levels of certain antibodies in their blood, which are substances that fight gluten.
Gluten sensitivity and celiac disease cause a lot of the same symptoms. But people with gluten sensitivity don’t have an abnormal gene or antibodies in their blood.
What’s The Difference Between Celiac Disease And Wheat Allergy
There are several different forms of protein in wheat that can cause allergic symptoms, including , the protein responsible for reactions in celiac disease and gluten sensitivity.
But a wheat allergy isn’t the same thing as celiac or gluten sensitivity: the conditions all involve completely separate components of your immune system and different types of reactions .
Technically, wheat allergy is a true allergy, while celiac disease is an autoimmune disease. People with true wheat allergy can usually eat the grains barley and rye, while people with celiac or gluten sensitivity must avoid those grains along with wheat.??
How Is Celiac Disease Treated
If you have celiac disease, you can’t eat any foods that contain gluten . You will be encouraged to visit with a dietitian for formal diet instruction. Dropping gluten from your diet usually improves the condition within a few days and eventually ends the symptoms of the disease. However, the villi usually require months to years to complete healing. It might take two to three years for the intestines to heal in an adult, compared to about six months for a child.
You’ll need regular medical follow-up visits and have to remain on this diet for the rest of your life. Eating even a small amount of gluten can damage your intestine and restart the problem.
Following a gluten-free diet means you cannot eat many “staples,” including pasta, cereals and many processed foods that contain gluten. There may also be gluten in ingredients added to food to improve texture or flavor and in some medicines. Some less obvious sources of gluten may include ice cream and salad dressing. Cross-contamination is another common source of gluten which happens when gluten-free foods come accidentally into contact with gluten.
If you have celiac disease, you can still eat a well-balanced diet. For instance, bread and pasta made from other types of flour are available. Food companies and some grocery stores also carry gluten-free bread and products.
You can also eat fresh foods that have not been artificially processed, such as fruits, vegetables, meats and fish, since these do not contain gluten.
What A Doctor Can Do
If you’re experiencing unusual symptoms and believe you might have CD, GS, a wheat allergy or another digestive condition, reach out to your healthcare provider . Your doctor can help pinpoint what ails you, refer you to the appropriate specialists and begin treatment to alleviate your symptoms. Avoid self-diagnosing your condition or eliminating gluten from your diet before your appointment, which could influence your test results, leading to a misdiagnosis and slower recovery.
And if your tests results reveal that you do not have a digestive issue related to wheat or gluten intake but you’re still cutting them out of your diet to slim down or for some other perceived health benefit, you may want to reconsider. While some people may find it impels them to choose healthier foods in general, there’s no real evidence that eliminating gluten will help you drop pounds or improve your overall wellbeing. What’s more, if you’re not careful, eliminating gluten could deprive you of valuable nutrients — especially fiber, but also iron and calcium. Many gluten-free foods are also loaded with added sugar, too much of which is unhealthy in itself.
In the end, the gluten decision is best left to you and your doctor — and with a little knowledge, you can make the right choice for your health.
This content originally appeared on Sharecare.com.
What To Eat And Avoid
Gluten occurs naturally in wheat, rye, and barley. Most cereals, grains, and pasta, as well as many processed foods, contain gluten. Beers and other grain-based alcoholic drinks can also contain it.
It is crucial to check labeling because gluten can be an ingredient in some unexpected products.
Foods that do not contain gluten include:
- meat and fish
- cereals such as corn, millet, sorghum, and teff
- pasta, bread, baked goods, and other products labeled “gluten-free”
A person can also eliminate gluten from recipes by substituting ingredients and sometimes by adjusting the time and temperature of baking.
In the past, experts recommended that people with celiac disease avoid oats. However, now suggests that moderate amounts of oats are generally safe, provided that the oats have not touched gluten during processing.
According to the , manufacturers must not label a food product as gluten-free unless it contains less than 20 parts per million of gluten — the lowest level that tests can reliably detect.
It is worth keeping in mind while traveling that regulations about labeling vary from country to country.
Many processed foods can contain gluten, including:
- canned soups
Read more about what a gluten-free diet contains here.
Celiac Disease: A Whole
When your doctor hears you say “gluten allergy,” she’s likely to think first of celiac disease, which occurs when your immune system mounts an attack on your small intestine in response to ingestion of gluten-containing foods.
Celiac disease affects about one in every 133 Americans.
There are many different symptoms potentially caused by celiac disease—every case is different, and in fact some people don’t have any symptoms at all. But there are some symptoms that appear frequently in people ultimately diagnosed with celiac disease, including:
- Diarrhea and/or constipation
- Rashes
- Depression and/or anxiety??
The absence of these symptoms doesn’t necessarily mean you can rule out celiac disease: as I said, some people have no symptoms at all, or suffer mainly from neurological symptoms .
Myth Vs Fact: Celiac Disease Vs Wheat Allergy
August 14, 2017
MYTH: Celiac disease is the same thing as a wheat allergy.
FACT: Celiac disease is not the same as a wheat allergy.
Although celiac disease may appear to be similar to a wheat allergy because of the need to avoid certain foods, these two conditions are entirely different, with different health effects and treatments.
Wheat contains a protein called “gluten” which is also in other foods, including rye and barley. Importantly, not all gluten-free foods are wheat-free. And not all wheat-free foods are gluten-free.
The term “gluten-allergy” can be confusing. Some people use this term to mean celiac disease, and some use this term to mean wheat allergy, and others use this term if they choose to avoid gluten for other reasons such as intolerance or preference. Clear communication about the type of reaction to wheat or gluten can inform the type of avoidance and treatment required. If you are not sure about the type of reaction you may have, please ask your doctor.
Bottom line: Celiac disease and wheat allergy are very different conditions with different health effects and treatments.
Medical content reviewed by: Dr. Julia Upton, MD, FRCP Clinical Immunology and Allergy
Help us educate your communities and share this mythbuster with them! Find more mythbusters at .
Someone Must Be Eating Gluten For Tests To Be Accurate

Basic screening for celiac disease includes a serum TTG IgA and total serum IgA. Total serum IgA needs to be done to rule out IgA deficiency which occurs in about 10% of celiac patients. If IgA deficiency is present, the TTG IgG must be used but is less accurate. Further testing may be needed in those situations.
Some labs include a DGP-IGA and EMA in their celiac screen/panel or do these tests as a reflex. The confirmatory test is an endoscopic biopsy. The biopsy is indicated if tests are positive and are required for diagnosis.
Of note, many celiac centers and practitioners follow a more extensive evaluation process involving screening antibodies, genetic testing, clinical response to a gluten-free diet, and endoscopy. These protocols and other testing algorithms are beyond the scope of this article.
Most Breads Crackers And Wraps
Most breads, crackers, and wraps contain gluten. The only way to know for sure is to read the ingredient list and check to see which grains are used.
If you have a gluten intolerance, avoid the following:
- white bread
- malt vinegar
- ketchup
As an alternative, you can make your own condiments from gluten-free ingredients or purchase ones that are certified gluten-free.
Getting Started With A Gluten Free Diet
The first step in switching to a gluten free diet is learning to identify foods that contain gluten. The next step is to begin incorporating gluten free foods into your diet. The best way to identify gluten free foods is to simply look for the “gluten free” label on the package, as you’ll see on every single product. Another way to identify gluten-containing foods is to check the allergen warning on the food label – if it lists wheat, there is a good chance that the product also contains gluten. There are, however, gluten-containing ingredients that do not contain wheat, so you’ll have to be very careful when choosing foods that aren’t labeled “gluten free”.
Here are some of the different words that suggest a food contains gluten:
- Wheat
Treatment Options For Celiac Disease
1. Go Gluten Free
First and foremost thing to do to reduce the problem of this disease is to go gluten-free. Gluten free diet is the only way you will be able to manage celiac disease. Here are some gluten-rich foods you must avoid.
- Malt
- Semolina
- Triticale
A dietician can help you plan your diet accordingly and help you with alternative diet options that are healthier for you in this condition. You also need to avoid food that are made up of gluten or have even slight amount of gluten in them. This can cancel out your majority of food options but is good for your health. Gluten can be present in medications, food items etc like-
- Over the counter medications
Nutritional And Dietetic Therapies
Exclusive enteral nutrition is a first-line therapy in pediatric Crohn’s disease with weaker data in adults.:331 Evidence supporting exclusive enteral nutrition in ulcerative colitis is lacking.:333
Nutritional deficiencies play a prominent role in IBD. Malabsorption, diarrhea, and GI blood loss are common features of IBD. Deficiencies of B vitamins, fat-soluble vitamins, essential fatty acids, and key minerals such as magnesium, zinc, and are extremely common and benefit from replacement therapy. Dietary interventions, including certain exclusion diets like the can be beneficial for symptom management. Dietary fiber interventions, such as psyillium supplementation , may relieve symptoms as well as induce/maintain remission by altering the microbiome composition of the GI tract, thereby improving regulation of immune function, reducing inflammation, and helping to restore the intestinal mucosal lining.
Here Are All Of The Details About Non
Do you know what non-celiac gluten sensitivity is and how it differs from Celiac disease? For many people, a gluten-free diet is the key to feeling well. While some of these individuals have celiac disease, others do not fit the criteria for this diagnosis. We caught up with registered dietitians and gluten-free diet experts Dr. Anne Lee, RD, LD, and Jessica Lebovits, RD, CDN, CNSC from the Celiac Disease Center at Columbia University Medical Center to learn more about this often-misunderstood condition. We also asked Melissa Halas, MA, RDN, CDE about the clients she works with who benefit from a gluten-free diet.
How Would You Diagnose This In Practice
Most of the literature uses double-blind, placebo-controlled crossover trials to determine who actually has a response to the reintroduction of gluten and who may be responding to something else in wheat or food. A few different approaches are commonly taken:
- In some respects, a diagnosis of non-celiac gluten sensitivity is a diagnosis by default as currently there are no definitive tests or diagnostic criteria for the condition.
- In practice, patients undergo a complete diagnostic workup with their gastroenterologist. Testing is done to determine whether patients have celiac disease or wheat allergy through lab work and an endoscopy if there is suspicion for celiac disease.
- If these diagnoses are ruled out, a diagnosis of non-celiac gluten sensitivity can be made by the gastroenterologist.
Managing Food Allergies In Children
Because fatal and near-fatal wheat allergy reactions, like other food allergy symptoms, can develop when a child is not with his or her family, parents need to make sure that their child’s school, day care or other program has a written emergency action plan with instructions on preventing, recognizing and managing these episodes in class and during activities such as sporting events and field trips. A nonprofit group, Food Allergy Research & Education, has a list of resources for schools, parents and students in managing food allergies.
If your child has been prescribed an auto-injector, be sure that you and those responsible for supervising your child understand how to use it.

