How Can You Be Exposed To Latex
You can get exposed to latex:
- Through the , such as when you wear latex gloves
- Through mucous membranes, such as the , mouth, , and rectum
- Through inhalation. Rubber gloves can contain cornstarch powder, which absorbs the latex and can become airborne when the gloves are removed.
- Through the . This can happen when some medical devices containing rubber are used.
What Is A Skin Prick Test
This common test might be a little uncomfortable, but it isn’t painful. Your provider puts a small amount of latex on your skin and scratches or pricks the skin with a needle. Scratching the skin allows a bit of latex to get under the surface.
If you’re allergic to latex, the area will become red and itchy. You may develop raised welts called wheals . The skin irritation and wheals show that your immune system is reacting. It usually takes about 15 to 30 minutes for a reaction to occur.
Types Of Reactions To Latex
There are three different kinds of adverse reactions to latex, although they do overlap to a certain degree. These include:
- irritant dermatitis – characterised by crusty skin lesions. Irritant dermatitis isn’t the same as latex allergy, because it can be caused by a wide range of other factors, including washing with harsh soap or the action of sweat inside rubber gloves. However, irritant dermatitis is often a starting point for the development of latex allergy. Broken skin allows the absorption of latex. Without intervention, people with genetic susceptibility will progress from irritant dermatitis to latex allergy
- allergic contact dermatitis – this skin problem is caused by a reaction to the chemicals added to latex during manufacture, not to the latex proteins themselves. Typically, symptoms tend to develop after exposure. Once again, this is not true latex allergy. However, the absorption of latex through broken skin can increase the risk of latex allergy in susceptible people
- immediate-type latex allergy – in genetically susceptible people, initial exposure to latex prompts the immune system to create antibodies. On subsequent exposure to latex, the body mounts an immune system response, which includes the release of histamine. This can cause a wide range of sudden reactions including hives, swollen lips and, in severe cases, anaphylaxis. Anaphylaxis, or anaphylactic shock, is an emergency and can be fatal. In an emergency call 000 for an ambulance.
What Should I Do If I Have Latex Allergy
If you have an IgE-mediated latex allergy, work with your doctor to learn how to recognize anaphylaxis and how to treat it.
Prevent Allergic Reactions to Latex:
- Avoid latex. The only treatment for latex allergy is to prevent any contact with latex products.
- Get a letter about your latex allergy from your doctor.
- Ask co-workers to wear only non-latex gloves.
- Ask doctors, dentists and others health care workers to use latex-free gloves.
- Check labels to make sure products do not contain latex. Do not assume “hypoallergenic” products are latex-free.
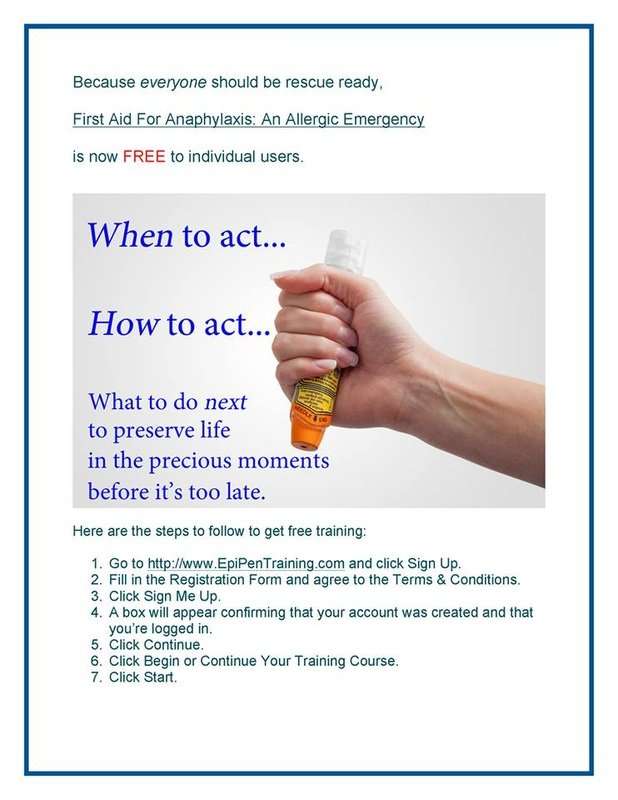
Prepare for Anaphylaxis Due to Latex:
- Have a written anaphylaxis action plan. Your doctor will give you this step-by-step plan on what to do in an emergency.
- Learn how to self-inject epinephrine . It is the medicine of choice to treat an allergic reaction or anaphylaxis. Epinephrine is safe and comes in an easy-to-use device called an auto-injector. It injects a single dose of medicine when you press it against your outer thigh. Your doctor will show you how to use it. Epinephrine can save your life if you have a severe reaction. After using an epinephrine auto-injector, you must immediately call 911 and seek medical care.
- Always have two epinephrine auto-injectors near you at all times.
- Teach people who spend time with you how to use the auto-injector device.
- Wear medical alert identification or jewelry to tell others of latex allergy in an emergency.
Is There A Connection Between Latex Allergy And Foods
Some rubber proteins are similar to food proteins. Therefore, some foods may also cause an allergic reaction in people who are allergic to latex. The most common of these foods are banana, avocado, chestnut, kiwi fruit, and passion fruit. Although many other foods can cause an allergic reaction, avoiding all of them might cause nutrition problems. Therefore, it’s recommended that you avoid only the foods that have already given you an allergic reaction.
What Causes Latex Allergy
Latex products are everywhere. Anyone can develop a latex allergy. Health care workers and rubber industry workers seem to have the highest risk for latex allergy. Health care workers who have hay fever have an especially high chance of developing a latex allergy. This is because 25% of all health care workers who have hay fever show signs of being sensitive to latex.
Other people at higher risk for latex allergy are:
- People who have had many operations
- People who have spina bifida
- People who have a food allergy
How We Can Help
Allergy Partners physicians are board certified experts in the diagnosis, treatment, and management of allergic diseases, including latex allergy. If you are having symptoms suggestive of latex allergy, your Allergy Partners physician will take a detailed history, perform a physical exam, and order appropriate testing to confirm the diagnosis of latex allergy or contact sensitivity. Working together, you and your Allergy Partners physician will develop a comprehensive and personalized treatment plan.
Who Is Likely To Have A Latex Allergy
Less than 1% of people in the US have a latex allergy. Although latex allergy is rare, the condition is more common in certain high-risk groups.
The highest risk is in children with spina bifida. Spina bifida is a condition in which the spine fails to form completely before birth. More than three out of every five children with spina bifida are allergic to latex.
Children who have frequent medical treatments or lengthy surgeries are also at high risk. Many medical supplies use latex – from gloves to tubing to enema tips.
Between 8 to 17% of health care workers and others who regularly use latex gloves are allergic to latex. Health care workers and children who have other allergies and get contact dermatitis when they use latex gloves are more likely to develop a latex allergy.
New cases of latex allergy are no longer common. However, in the 1980s and 1990s they were much more frequent. Now, many health care facilities use non-latex gloves and products.
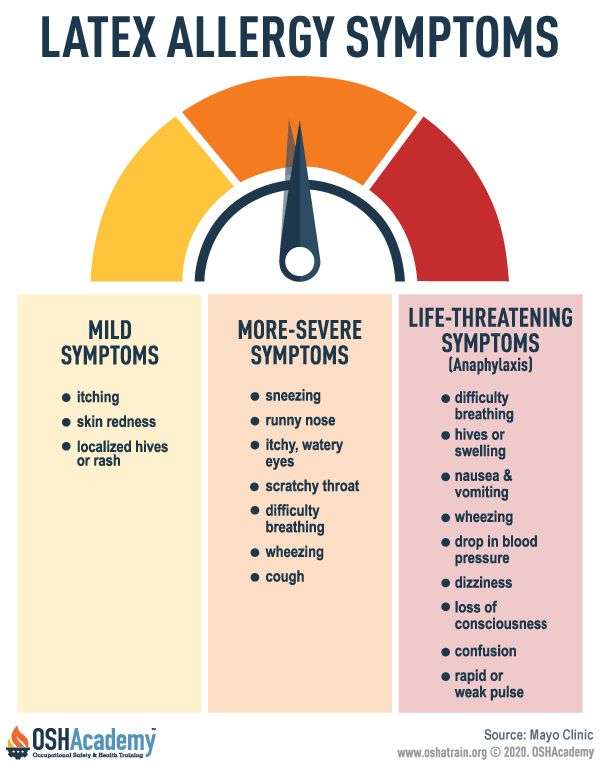
Latex Type I Allergy: Immediate Response
Symptoms range in severity, from mild discomfort to life threatening responses
- Low: Swelling and redness usually local to the site of exposure; non-specific symptoms include itching and burning
- Medium: Conjunctivitis, rhinitis, bronchial obstruction
- High: In rare cases, anaphylaxis can occur
RECOMMENDATION: Minimize the risk to sensitization or an adverse latex allergic reaction by switching to synthetic gloves.
What Are Symptoms Of Latex Allergy
Latex allergy symptoms range from skin irritation to respiratory symptoms to life-threatening anaphylaxis – and there’s no way to predict which will occur if exposed.
Symptoms of latex allergy may be mild at first, progressing to more serious types of symptoms.
Symptoms of latex allergy include:
- skin redness
- asthma
A latex allergy reaction can also result in anaphylaxis, a life-threatening allergic reaction.
Symptoms can start within seconds of exposure to latex or may not appear until hours later. The allergic reaction can be different each time a person experiences anaphylaxis and can vary in severity each time. Once the reaction starts, it usually progresses quickly. This makes identifying anaphylaxis and responding to care tricky at times.
A board-certified healthcare professional, often an allergist, makes the diagnosis of latex allergy, as well as contact dermatitis and/or irritant dermatitis. The healthcare professional uses a combination of medical history, physical exam and various laboratory and clinical tests. Laboratory testing alone is not enough to make a diagnosis.
Patients are encouraged to provide a full list of items and foods that may have caused a latex-allergic reaction to help determine whether latex allergy is present.
Allergy Asthma & Immunology Specialists Located In Scottsdale Az & Gilbert Az
A latex allergy is rare but potentially deadly. It’s important to take latex reactions like skin redness, swelling, and itchiness seriously and see the expert allergists at Allergy, Asthma & Immunology Associates, LTD. The team of specialists has a 50-plus year history of helping Arizonans with all their allergy needs. Call one of the locations in Scottsdale or Gilbert, Arizona, or schedule an appointment online.
- Request an Appointment
What Are Important Things To Know About Latex Allergy And Schools
Providing a safe environment for students at school goes beyond food and environmental allergies – latex allergy must also be considered. In the school setting, we often see latex allergies in children who have experienced multiple medical procedures, especially children with spina bifida.
Latex appears in items commonly used in school, including many brands of erasers, balloons, rubber bands, gloves, balls and mats used in physical education. The school needs to identify latex-free school products and latex-free sports equipment when a student has an allergy.
All members of the school community should collaborate to manage latex allergy by:
- Educating the school community
What Products Contain Latex
Latex is often found in medical and dental offices, but can also be found in your home. Common latex products include:
- Disposable gloves in medical or dental offices
- Medical adhesive tapes used for dressing wounds
- Catheters
- Mouse pads for computers
- And more
If you experience reactions to these or other products containing rubber latex, it’s best to avoid contact whenever possible.
Routes Of Latex Exposure
Latex exposures can occur through direct contact with the skin, mucous membranes, or bloodstream, and through inhalation of airborne latex particles. The protein responsible for latex allergies has been shown to fasten to powder that is used on some latex gloves. When powdered gloves are removed, latex protein/powder particles get into the air, where they can be inhaled and come in contact with mucous membranes in the eyes, nose, and mouth.
Parenteral exposures are those in which latex may enter the bloodstream directly. These exposures have the potential for the most serious reactions. Parenteral exposure can occur during surgery when latex devices are used on open tissue. It can also occur following injections with needles that have punctured a latex rubber stopper on a medication vial.
Inhalation of airborne latex particles can occur when latex proteins combine with the powder or cornstarch from the gloves and form aerosolized particles that become airborne. These particles get into eyes, nose, mouth, or lungs, where protein may be absorbed through these moist mucous membranes.
To ensure safety, in February 2011, the FDA recommended adding a warning label to exam gloves containing powder on their potential health effects.* FDA’s suggested warning for surgical and exam gloves states the following:
What Are Important Things To Know About Latex Allergy And Vaccines
Some vaccine packaging contains latex, posing a threat to people who have a latex allergy. There is concern that latex proteins may be mixed with the medication through packaging and storage of the vaccine vial, and also through puncturing the vial stopper to “draw up” the vaccine. The same concern exists with vaccines that are stored in syringes with latex in the plungers.
While the extent of the risk is unknown, it is difficult to be sure how much latex may be present in a vaccine package. Since current recommendations are based on limited data, patients should talk with their allergists to determine the best approach to obtaining a needed vaccine.
Current strategies can include:
- “Popping the top” prevents the puncturing of a latex stopper for safer administration. However, there is still a possibility that latex allergic proteins contaminated the medicine during the period of storage.
- The “one stick rule” is based on the assumption that a single stick through the vial seal minimizes latex allergen distribution into the medication, while maintaining a closed system that limits potential for contamination.
- Post-vaccination observation by a qualified individual for a period of at least 15 minutes, and up to two hours.
What Do You Do If You Have A Latex Allergy
- Wear Medical Identification
- Carry with you at all times:~ Medications, as prescribed by your allergist ~ Non-latex gloves
- ~ “Hidden” latex on food prepared with latex gloves Lactiferous plants that may have cross-reactive proteins ~ Foods with cross-reactive proteins to natural rubber
- Carry a list of medications prescribed by your allergist
Symptoms Of Latex Allergy
The symptoms range in severity depending on the individual, but can include:
- dermatitis
- lesions that are irritated by sweat and friction
- hay fever symptoms, such as running nose and itchy eyes
- sneezing
- wheezing and breathing difficulties
- drop in blood pressure
- anaphylaxis or anaphylactic shock – severe symptoms include airways swelling to the point of suffocation. Anaphylaxis is an emergency and can be fatal. In an emergency call 000 for an ambulance.
Can Latex Allergy Be Prevented Or Avoided
If you are a health care worker or a patient, everyone around you should wear powder-free latex gloves or non-latex gloves. If you are a health care worker, compare different kinds of non-latex gloves to find the ones that are best for you.
Always wear or carry a medical alert bracelet, necklace, or keychain. This will warn emergency medical technicians and doctors that you are allergic to latex. Talk to your doctor about getting a prescription for an epinephrine self-injection pen. You will use this pen in case of a serious reaction. You may wish to carry non-latex gloves with you all the time. Emergency personnel can use these if you need medical attention.
If you are exposed to latex at your job, tell your employer and co-workers about your latex allergy. Avoid latex gloves completely if you’re not at risk for blood and body fluid contamination. Use powder-free gloves if latex gloves are preferable. These measures will help keep others from becoming allergic to latex.
Latex Allergy Immune Response
A latex allergy, also called latex sensitivity or Type I latex hypersensitivity, is an immune response following exposure of genetically predisposed individuals to the proteins in natural rubber latex. These latex proteins are the specific substances or allergens that can simulate the allergic response. More than 200 latex proteins exist, and more than 50 may have the potential to cause allergic reactions.
A person with a potential for developing a latex allergy will have an immune response when first exposed to latex, although no external or physical response may be noted . The immune response initiates production of latex-specific antibodies or immunoglobulins that take part in the development of symptoms when a person is re-exposed to latex These antibodies are also helpful in diagnosing a latex allergy.
An individual with an allergy to latex becomes increasingly “sensitized” with each subsequent exposure, increasing the potential for the development of a reaction following exposure These symptoms can range from itching to the most severe and potentially fatal reaction , a collapse of the cardiac and respiratory system. The amount of latex exposure needed to produce sensitization or an allergic reaction is unknown However, reductions in exposure to latex proteins have been reported to be associated with decreased sensitization and symptoms.
People At The Greatest Risk For A Latex Allergy
The number of healthcare workers affected by latex allergies is much higher than average. In fact, the Asthma and Allergy Foundation of America estimates that between 8 and 17 percent of all healthcare workers have the allergy. The increased use and exposure to latex is thought to be the main reason for the higher rates in this group.
Others who are at increased risk include:
- those with food-related cross-allergies
What To Do About It
And if the problem persists, you’ll have to stop by your gynecologist’s office. The only way to truly rule out either a stubborn yeast infection or a latex allergy is to test for it. “You’ll need to see a specialist in vulvovaginal disorders or an allergist to get to the bottom of the situation, once your doctor has ruled out other causes,” Shepherd says. If it turns out that latex is the culprit, you have a few options .
“ are thinner but stronger than latex, and they transfer heat more efficiently, which may enhance sensation,” Shephard says. And there are newer , which are a more flexible option that many find to be a comfortable fit .
Irritant Dermatitis And Potential Latex Allergy
If you have irritant dermatitis, you can reduce your risk of developing latex allergy in a number of ways including:
- Choose synthetic rubber products if possible.
- If you have to wear latex gloves, ask for the non-powdered variety .
- Request that your co-workers also wear non-powdered gloves.
- Wash hands thoroughly after wearing latex gloves.
- Take care of your hands to ensure an unbroken skin surface.
- Always have skin rashes medically investigated.
- Consider alternative forms of contraception to condoms or diaphragms. Non-latex condoms can be used for barrier protection from sexually transmitted infections.
How Do You Treat A Latex Allergy Reaction
Latex allergy treatment depends on the type of reaction that is present – a mild sensitivity or a life-threatening allergic reaction, or anaphylaxis.
- Anaphylaxis: Epinephrine, a medication given by injection that works quickly to raise blood pressure and reduce swelling in the body, is the first-line treatment for severe allergic reactions. It’s available in an easy-to-use epinephrine auto-injector – a prefilled syringe with a retractable needle. Epinephrine should be administered without delay when symptoms appear.
- Mild Sensitivity: If a mild sensitivity is present and there is only a local reaction – the skin is itchy and red at the site where latex was touched – your doctor may suggest using an antihistamine or using 1% hydrocortisone cream.
NOTE: Treatments mentioned here are for informational purposes only. If you have a latex allergy and require treatment, you should see a board-certified allergist to determine the best treatment for you.
What Is A Cross
Some people who are allergic to latex may also be allergic to specific foods – we call this a cross-reaction. In short, the body’s immune system responds to a food item, producing the same allergic symptoms as would occur with exposure to latex.
Cross-reactions are not the same for all people. While some people react to all foods known to cause a cross-reaction , others may not. In the same way, if someone is allergic to any of the foods listed below, they might also be allergic to latex:
Some fruits – strawberries, pineapple, pears, nectarines, cherries, passionfruit, , melons, grapes, figs, plums, peaches, kiwi, bananas, and apples.
Vegetables – tomatoes, avocados, celery, carrots, and raw potatoes.
Some nuts – hazelnuts and chestnuts.
Some cereals – rye and wheat.
Anybody planning to undergo a medical procedure should tell their doctor if they are allergic to any of these foods. There is a risk they may have a cross-reaction to latex.
Treatment Of Latex Allergy
There is no cure for latex allergy. Repeated exposure to latex can escalate the immune system response, so avoidance is the best way to manage the condition.
Suggestions include:
- Choose synthetic rubber products.
- You may have to change career if your profession involves unavoidable exposure to latex.
- Consider alternative forms of contraception to condoms or diaphragms. However, remember that condoms are essential as barriers against sexually transmitted infections. Latex-free condoms are available from pharmacists and other retailers.
- Always tell your health care professionals that you are allergic to latex before undergoing any procedure, so they can make sure to have non-latex equipment on hand.
- Be on the lookout for situations that may expose you to latex – for example, your hairdresser or take-away food handler may wear latex gloves.
- Avoid foods that trigger symptoms.
- Wear a specially designed medical alert bracelet or pendant to provide information about your allergy in case of emergencies.
- If prescribed, always carry an adrenaline autoinjector in case you experience anaphylaxis.
- Make sure that family, friends and co-workers know how to use the adrenaline autoinjector .
What Is Latex Allergy
Latex allergy is a reaction to certain proteins in latex rubber. The amount of latex exposure needed to produce sensitization or an allergic reaction is unknown. Increasing the exposure to latex proteins increases the risk of developing allergic symptoms. In sensitized persons, symptoms usually begin within minutes of exposure; but they can occur hours later and can be quite varied. Mild reactions to latex involve skin redness, rash, hives, or itching. More severe reactions may involve respiratory symptoms such as runny nose, sneezing, itchy eyes, scratchy throat, and asthma . Rarely, shock may occur; however, a life-threatening reaction is seldom the first sign of latex allergy.
Wear A Medical Bracelet
If you have severe allergies or are prone to anaphylaxis, it’s a good idea to wear medical alert jewelry to alert others around you of your condition. The MedicAlert Foundation offers several options including medical bracelets, dog tags, watches, sports bands and other types of identification. The foundation can notify friends and family in the event of an emergency. The service is available 24 hours a day, 7 days a week.
Tree Nuts Seeds And Soy
Tree nuts, legumes and seeds are common offenders for people who have severe food allergies. Peanuts are one type of legume. Lentils, chickpeas, peas and soy are also in the legume family and may provoke allergic reactions. Tree nuts including cashews, almonds, Brazil nuts, walnuts and macadamias can also trigger allergic reactions. Seeds like sesame seeds, poppy seeds, sunflower seeds and pumpkin seeds may trigger food allergies. Coconut is another seed that people can be allergic to.
Latex Allergy Symptoms And Diagnosis
Common latex allergy symptoms can range from minor to life-threatening. These symptoms may include:
- Rash, inflammation, hives, or itching on the skin
- Mild respiratory reaction: coughing, sneezing, or a runny nose
- Severe respiratory reaction: shortness of breath, swelling of the throat, or wheezing
- Anaphylaxis, a life-threatening allergic reaction requiring immediate medical attention
Symptoms often occur within minutes after contact with the allergen. Most symptoms occur after direct contact with latex. In other cases, inhaling latex proteins in the air can cause asthmatic reactions in latex allergy sufferers.
Connection Between Food Allergy And Latex Allergy
Certain fruits contain the same allergens found in latex. They include:
- Avocado
- Surgical masks
- Dental dams
Many health care facilities use nonlatex gloves. However, because other medical products may contain latex or rubber, be sure to tell doctors, nurses, dentists and other health care workers about your allergy before all exams or procedures. Wearing a medical alert bracelet can inform others of your latex allergy.
What Are The Signs Of A Latex Allergy
A latex allergy can cause symptoms such as:
- Red skin
- Nasal symptoms like runny nose or sneezing
- Red eyes
- Difficulty breathing
Latex allergies can potentially cause anaphylaxis, a severe whole-body reaction that may include rash, vomiting, breathing problems, chest pain, fainting, and shock. Anaphylaxis can be deadly, so fast reaction time is critical if you suspect a latex allergy.
Questions To Ask Your Doctor
- Latex is a rubber product. Am I at risk for other rubber allergies?
- What products contain latex? How do I avoid these?
- How do I make sure that all members of my health care team know about my latex allergy?
- How do I know if my allergic reactions are getting worse?
- Could I be at risk for anaphylaxis? Do I need to carry epinephrine?
- Do I need a medical alert bracelet? Where do I get one?
- I’m sexually active. What’s a good alternative to latex condoms?
What Are The Symptoms Of Latex Allergy
Signs of an allergic reaction to latex can be mild or severe. They can appear right after exposure to latex or up to a few hours later. You might not have symptoms the first time you come into contact with latex. Latex allergy symptoms include:
- Skin irritation: Itching, inflammation, redness and swelling appear after skin contact with latex. For example, you may have itchy lips after blowing up a balloon or vaginal irritation after having sex with a partner who used a latex condom.
- Rash: An itchy rash appears where the latex touched your skin. A latex allergy rash usually occurs within a day after exposure. The rash can spread if it touches skin on other parts of your body. But you can get a rash from other factors, such as using too much hand sanitizer or washing your hands too often.
- Hives, runny nose and sneezing: Itchy, watery eyes and inflammation around the nose and mouth are common. Eyes may become swollen and red.
- Trouble breathing: People who have severe allergic reactions may wheeze or have difficulty breathing. In severe cases, may occur. Anaphylaxis can be fatal. If you or someone you know is having an allergic reaction and can’t breathe, call 911 or go to the emergency room.

