Can Allergies Cause Inflammation In The Lungs
allergiccauses inflammationlungsallergiccan cause lung
. Also question is, what can cause inflammation in the lungs?
Pneumonitis occurs when an irritating substance causes the tiny air sacs in your lungs to become inflamed. This inflammation makes it difficult for oxygen to pass through the alveoli into the bloodstream. Many irritants, ranging from airborne molds to chemotherapy drugs, have been linked to pneumonitis.
how do you get rid of inflammation in the lungs? Fatty fish like salmon, mackerel, tuna and sardines: high in omega-3 fatty acids, which can help reduce inflammation. Fruits such as strawberries, blueberries, cherries and oranges: rich in vitamin C and vitamin B6 helps the lungs transfer oxygen.
Regarding this, can allergies cause chronic inflammation?
Chronic allergic inflammationWhen allergen exposure is continuous or repetitive, inflammation persists, and many innate and adaptive immune cells derived from the blood can be found in the tissues at sites of allergen challenge.
Can allergies cause respiratory infection?
Acute bronchitis usually goes away after a few days or weeks. Allergic bronchitis is chronic, and may be caused by exposure to allergy triggers like tobacco smoke, pollution, or dust. You may also hear it called chronic bronchitis. People with bronchitis often cough a lot and have trouble breathing.
How Are Interstitial Lung Diseases Diagnosed
Doctors will perform a physical exam and evaluate your family medical history. They may also seek to rule out diseases that have similar symptoms.
Diagnostic tests that search for inflammation and/or scarring in the lungs may include:
- Lung function testing
- Bronchoscopy to examine the lungs or get a tissue sample
Allergen Sensitization And Epithelial Barriers
Sensitization to an allergen reflects the allergens ability to elicit a TH2-cell response, in which IL-4 and IL-13 drive IgE production by promoting immunoglobulin class-switch recombination in B cells,,,, .
Sensitization to allergens in the airway
Many factors affect the likelihood of developing clinically significant sensitization,: host genotype, type of allergen, allergen concentration in the environment and whether exposure occurs together with agents that can enhance the sensitization process. These agents include certain ligands of Toll-like receptors, including endotoxin, which can promote TH1-cell responses and in certain circumstances might be able to enhance the development of TH2-cell responses. Other agents that can enhance allergic sensitization are chitin, which is found in many organisms , and environmental pollutants. Another important factor is the pattern of contact of the immune system with allergens: for example, the amount, frequency and/or route of allergen exposure and the type and phenotypic characteristics of the dendritic-cell subpopulations that participate in the responses. The pattern of contact may affect whether there is a strong TH2-cell response , a TH2-cell response that is kept in check by IL-10-secreting, and perhaps other, regulatory T cells,,, a modified TH2-cell response that results in high concentrations of allergen-specific IgG4 or another form of immunological tolerance.
You May Like: Allergies Cause Tiredness
Air Pollution And Hypersensitivity Pneumopathy
PHS are non-IgE mediated immuno-allergic pathologies, secondary to repeated exposure to organic antigens. There is a wide variety of environmental agents responsible for this pathology, which occurs in people who are probably predisposed. PHS can occur in a domestic or occupational context .
An Indian team carried out an epidemiological study that identified all new cases of PHS from 27 centers in 19 cities in India from 2012 to 2015. From 1084 new ILDS cases, they found that 78% were in urban areas and 43% were PHS . This prevalence of PHS in ILDS is surprisingly much higher than those previously reported in the literature . Because of the high exposure to pollution in India, the authors assessed its potential role in the incidence of PHS . A positive correlation between the percentage of PHS cases and PM2.5 levels was found, with, for every 10 g/m3 increase in PM2.5 level, a 7% higher risk of developing PHS compared to other ILDS, even after adjustment for domestic and occupational PHS exposures. The authors hypothesize that air pollution may mediate the retention and awareness of the antigen responsible for PHS .
Karen C. Patterson MD, Cecile S. Rose MD, MPH, in, 2016
How Does Hypersensitivity Pneumonitis Develop

Hypersensitivity pneumonitis does not develop on the first day of exposure to animal and vegetable dusts. Repeated and prolonged exposure is necessary. Even then, only some workers develop allergic reactions to the dusts. Ten to forty percent of exposed people do not show any symptoms.
The allergy is triggered by complicated reactions of the body’s natural defense system that normally protects the lungs from foreign substances. In some individuals, the chemical reactions of the defense system that would ordinarily protect the lungs actually cause the inflammation and lung damage. The body’s changing response to the presence of dust in the lungs is called sensitization.
You May Like: What Allergy Medicine Is Stronger Than Zyrtec
Treatments For Inflammation In Lungs
Lung inflammation treatment totally depends upon the cause of the inflammation and the type of symptoms experienced. There are many tests which help in finding out the cause behind the inflammation. X-ray and CT scan are some of the most important imaging tests which gives detailed information about the organ. Saturation of oxygen in the blood is also done in order to check out the proper functioning of lungs with the help of oximeter.
Then according to the diagnosis following treatments may be prescribed by the doctor.
- Antibiotics are prescribed in case of infections which are caused due to microorganisms. The dosage and the type of antibiotics will depend upon the microorganism responsible for the infection.
- Inhalers may be an effective treatment for allergies. The symptoms may be cured but the disease may take a longer time to be cured or may reappear after sometime.
- In worst cases, the doctor may advice a fluid drainage for the patient. With the help of this method, the mucus which is collected in the lungs is drained with the help of a machine.
The people who are suffering from lung inflammation should avoid exposure to smoke, dust and pollution. Smoking can be very dangerous, hence, should be stopped immediately once the condition is diagnosed. Maintain a proper healthy diet, take proper rest and follow your physicians instructions carefully. These precautions will reduce the chances of complications and will help you to recover fast.
Ige And The Exacerbation Of Allergic Disorders
Many patients who initially have a single allergic disorder, such as atopic dermatitis, eventually develop others, such as allergic rhinitis and allergic asthma . This process may be driven in part by a vicious circle in which allergic inflammation diminishes the function of the epithelial barrier. This increases the immune systems exposure to the original allergens and additional allergens, and existing allergen-specific IgE contributes to sensitiz ation to new allergens. In this scheme, antigen-presenting cells that express surface FceRI and/or the low-affinity IgE receptor CD23 capture allergens by means of their surface-bound allergen-specific IgE. By processing these IgE-bound antigens, APCs can promote the development of TH2-cell responses to other epitopes of the allergen for which sensitization already exists or to other allergens that are being processed in parallel by the same APCs. This proposed mechanism may result in epitope spreading .
In this model, the acquisition of IgE-dependent immunological reactivity to more and more allergens would occur in parallel with the clonal expansion of populations of effector T cells that can respond to any of a group of allergen-derived peptides. However, a diverse range of genetic and environmental factors can influence the extent to which the pathology in individual allergic subjects depends on allergen, allergen-specific IgE, FceRI, mast cells and basophils, as opposed to allergen-derived peptides and effector T cells .
Read Also: Can Seasonal Allergies Make You Throw Up
What Should I Know About Ipf
- Every person diagnosed with pulmonary fibrosis has a unique experience with the disease. Some patients remain in stable condition for extended periods of time others may experience a rapid progression of symptoms while another group may experience a stepwise deterioration over time.
- Symptoms include shortness of breath, dry cough, fatigue, unexplained weight loss, aching muscles and joints as well as clubbing of the fingers or toes.
- There is no cure for IPF. The average life expectancy of someone with pulmonary fibrosis is 3-5 years but if its caught early, treatment can help slow the progression of the disease.
- Treatment is highly personalized, based upon a patients medical history and other conditions. Medications are available to help slow the progression of the disease. Oxygen therapy and pulmonary rehabilitation may also help. For the most severe cases, a lung transplant may be considered.
Airway And Vascular Responsiveness In Isolated Perfused Mouse Lung
After a steady state period of 30min, 5-HT or, alternatively, the thromboxane receptor agonist U46619, angiotensin II or endothelin-1 were administered to the perfusate for 30s, 3, 2 or 10min, respectively. The concentration of either agent was increased in 12-min intervals. Raw and Ppa were determined 30s before and at the respective maximum response after 5-HT, U46619, angiotensin II or endothelin-1 administration. The change in Raw was expressed as fold Raw, and the difference in Ppa was expressed in cmH2O.
Ketanserin , GR127935 , D609 , xestospongin C , bisindolylmaleimide , or Y27632 were administered to the perfusate 10 min prior to 5-HT application.
Recommended Reading: Keflex Amoxicillin Allergy
What Is Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis is a lung disease causing inflammation of the lung tissue. This inflammation makes breathing difficult. It can lead to irreversible lung scarring over time.
HP results from breathing in specific environmental allergens. Allergens are substances that cause an allergic reaction in the body. These allergens may be present at home, at work, or in nature. Bird feathers and droppings, and household mold are examples of common allergens.
Do Antihistamines Thicken Mucus
antihistamineAntihistaminesthicken mucusTaking the following actions can help to eliminate excess mucus and phlegm:
Don’t Miss: Antihistamines Hypertension
Phlegm Or Sputum: Whats Normal
- Yellow or green phlegm is a normal part of the healing of viral bronchitis.
- This means the lining of the trachea was damaged by the virus. Itâs part of the phlegm your child coughs up.
- Bacteria do not cause bronchitis in healthy children. Antibiotics are not helpful for the yellow or green phlegm seen with colds.
- The main treatment of a cough with phlegm is to drink lots of fluids. Also, if the air is dry, using a humidifier will help. Sipping warm clear fluids will also help coughing fits.
Causes Of Chemical Pneumonitis
Any toxic or poisonous substance that can enter the lung may cause tissue damage and inflammation . These substances may be in gas, liquid or solid form. In terms of solids, only small particles like dust can pass down the airways and reach the lung tissue.
Sometimes non-toxic substances may trigger an allergic reaction in the lung but not directly injured the lung tissue. This is known as hypersensitivity pneumonitis. However, it is possible for toxic substances to both damage the lung tissue and trigger an allergic reaction.
Don’t Miss: Amoxicillin Benadryl
Inflammation: Your Immune System Under Stress
How can we get inflammation from foods? When the complex proteins casein and gluten break down in the digestive tract they form protein fragments that can be ‘mis-read’ by the body as foreign invaders. Once they are in the bloodstream – your immune system sends out the antibody cavalry, and the inflammation begins.
- Inflammation at the joints causes stiffness and arthritis
- Inflammation in the lungs or nasal passages causes respiratory congestion, asthma and chronic cough
- Inflammation in the membranes of the brain causes headache and migraine
- Inflammation in the nervous system causes neurological disorders like multiple sclerosis, epilepsy
- Inflammation at the skin can cause hives, eczema and psoriasis
But a simple switch in foods means the cause of the inflammation is removed – and the body begins healing naturally.
Toxins That Cause Chemical Pneumonitis
A host of different toxic substances may lead to chemical pneumonitis. Usually this is in the gas or vapor form but can also occur with liquids and small particulates. For most people the risk is within the home while for others it may be at the workplace. Common substances that cause chemical pneumonitis includes:
- Pesticides and herbicides.
- Drain cleaners acids like sulfuric acid fumers or alkalis such as ammonia.
- Chlorine swimming pool chlorine or bleach.
- Smoke from fires.
- Dust from fertilizer and grains.
- Oils and hydrocarbons paraffin, kerosene, gasoline and petroleum products.
Chemical spills, industrial pollution, very heavy smog and even agents used in chemical warfare may be responsible for chemical pneumonitis in the general population. A number of other substances may also cause chemical pneumonitis in the workplace. Workers who are not using protective gear or working in facilities with inadequate systems are at the greatest risk of both acute and chronic pneumonitis.
You May Like: What Allergy Medicine Is Stronger Than Zyrtec
What You Can Do At Home
To control or loosen mucus at home, you can try the following remedies:
Drink lots of fluids. Drink plenty of water and other fluids, but not things that can dehydrate you, such as coffee and alcohol.
Humidify. Try a cool mist humidifier or hop into a steamy shower to keep your airways moisturized.
Dont smoke or vape anything. Whether from tobacco or , smoke is an irritant and can cause your body to make more mucus.
Try a teaspoon of honey. Though honey doesnt get rid of mucus, it can calm your cough temporarily.
Check air filters. Other irritants in the air can make mucus production worse, so make sure your heating and cooling system filters are clean and up to date.
Take an expectorant. Some cough medicines contain guaifenesin, which loosens mucus so you can cough it up.
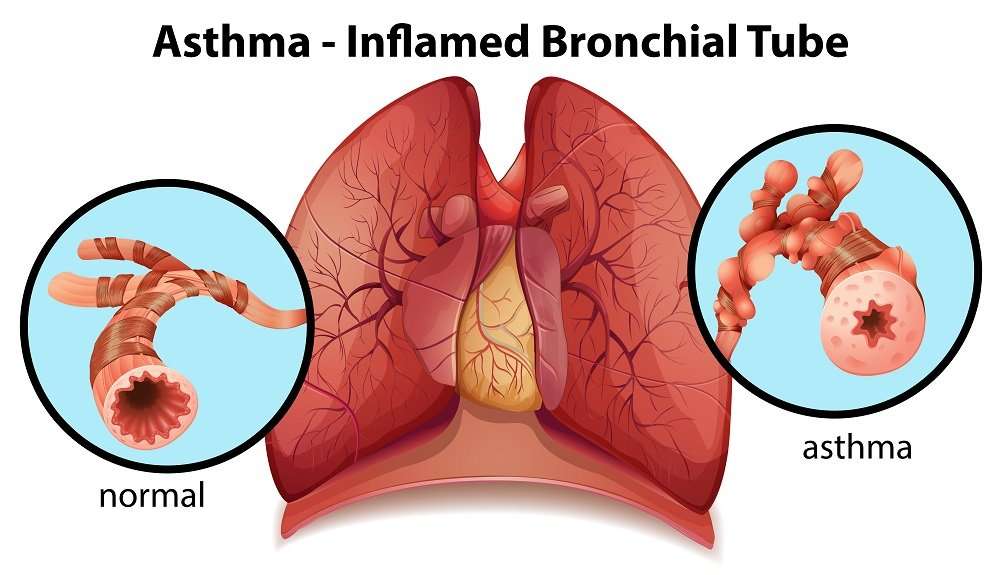
Changes In The Lower Airways In Asthma: Inflammation And Remodeling
Both inflammation and structural changes occur in the tracheobronchial tree of patients with asthma. It has been generally considered that chronic eosinophilic inflammation is a prerequisite for the development of remodeling, and there is some animal experimental evidence to support this . Investigations in humans to discover whether chronic inflammation leads to remodeling or whether remodeling begins first are in their infancy . Such studies are required so that we may determine if and when there may be a ‘window of opportunity’ for prevention of the structural and inflammatory changes associated with the asthma phenotype. Moreover, it may become possible to predict which preschool ‘wheezers’ will go on to develop asthma.
Chronic inflammation plus remodeling contribute to airway wall thickening, which encroaches upon the airway lumen and increases resistance to airflow . Airway secretions also contribute to the pathology of asthma, and especially to the consequences of acute, severe, life-threatening exacerbations. In those rare cases when a fatal asthma attack has occurred after a short duration of asthma, airway wall thickening may not be present and in these cases patient demise is assumed to be secondary to asphyxiation from tenacious, sticky mucus admixed with an inflammatory eosinophilic exudate in the airways .
Figure 1
Recommended Reading: Is Zyrtec Good For Itchy Skin
Constant Phlegm In Throat: 14 Causes Symptoms 13 Home Remedies
Constant phlegm in throat can irritate you a lot and you wont be able to concentrate on anything. So, lets learn how to get rid of it.
Phlegm is a thick sticky substance that is present in the throat. Also known as mucus, generally mucus in throat is associated with sickness but it is believed that some amount of phlegm is always present in the throat.
Tissues which secrete mucus are present in throat, GIT, nasal cavity, nose and lungs. Mucus acts as a protective covering for the tissues in throat, nose and GIT tract. It also helps in keeping the tissues and organs from drying by keeping them moist. Mucus is also the carrier of antibodies which help to fight against the external substances.
The normal amount of Phlegm is required in the body however, it is the presence of excess or constant phlegm in the throat that causes the problem, often irritates the person and also obstructs the respiratory passage. Some people react to certain external food substances such as milk and produces constant phlegm in throat.
Contents
Causes of Constant Phlegm in throat:
There are various reasons and causes associated with constant and excessive phlegm in the throat or a feeling where one feels that there is mucus in throat all the time. Some of the causes for constant phlegm in throat include:
Post-Nasal Drip:
This is characterized by mucus travelling from nose to throat usually happens due to an allergy to some food item.
Cold or flu:
Also Check: Can Allergies Make You Throw Up
Vinpocetine Alleviates Lung Inflammation Via Macrophage Inflammatory Protein
-
Roles Conceptualization, Data curation, Investigation, Methodology, Writing original draft
Affiliation College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea
-
Affiliation College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea
-
Roles Data curation, Formal analysis, Investigation, Methodology
Affiliation College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea
-
Roles Data curation, Formal analysis, Investigation
Affiliation College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea
Don’t Miss: Small Blisters On Lips Allergic Reaction
How Hypersensitivity Pneumonitis Affects Your Body
When you inhale the dust that you are allergic to, you wont notice any problems the first time. Some people develop symptoms after inhaling a lot the dust all at once or after inhaling small amounts over and over again. Tiny air sacs in the lungs can become irritated and may fill with fluid. If you stop inhaling the allergen, the irritation can get better in a few days. If you keep inhaling those allergens, the lung irritation continues. Parts of your lung can develop scar tissue. When your lungs have scar tissue, it may be hard to breathe normally.
Its important to catch this disease early so that you dont have permanent lung damage:
- Hypersensitivity pneumonitis can be a serious problem for people whose lungs become scarred.
- Scarred lungs can occur if the disease continues, and it is permanent.
- Unfortunately, there is no cure or treatment for long-term hypersensitivity pneumonitis.

