Vi The Headache Threshold
Understanding the concept of the headache threshold is the key to understanding why migraine patients experience more frequent and severe headaches. Everyone has the ability to experience a headache and, in fact, it can be an important warning sign for many disorders. Your bodys headache threshold is the point at which certain conditions in your body initiate headache symptoms. Migraine patients have a much lower threshold than those who do not experience frequent headaches.
Consider this bathtub analogy:
The top of the bathtub represents your headache threshold. When water reaches the top of the tub, it begins to overflow, symbolizing your threshold being crossed. Migraine patients have a much smaller bathtub and are more likely to experience headaches from events or physical changes that would not cause a headache in others.
Now picture the bathtub with many faucets emptying into it at varying and alternating rates. For migraine patients, these faucets represent headache triggers. The faucet that causes the overflow can vary from one day to the next, just as the migraine trigger to breach your headache threshold varies. The strength and sum of these triggers determines the frequency and severity of your migraine headache.
Diagnosing And Treating Food Associated Headaches
Diagnosing a food allergy headache is extremely difficult. While there is testing for food allergies, they are not very accurate giving a false positive result about 40 to 60 percent of the time.
Other ways to diagnose food allergy headaches include an elimination diet or food challenge. An elimination diet involves removing all possible food triggers from the diet and adding them back into the diet one at a time and recording the result. When a trigger is found, it is removed, and the elimination diet continued to determine other triggers.
A food challenge entails giving the person increasing amounts of a food that is thought to be a trigger until a reaction occurs. This type of test is considered the most accurate way to check for a food allergy.
A food diary is another way to check for food-related triggers and is a common practice in any migraine clinic. When you get a headache, you write down what you ate prior to the headache along with any symptoms or auras you had before the migraine or headache. This makes it easy to track foods and food combinations that may be triggers. A food diary can be an excellent ally for tension headache treatment as well as chronic headache treatment.
Also Check: Medicine Claritin
How Do Allergies Cause Migraine Headaches
The link is complex. Doctors are still trying to figure it out. So far, they know that your nervous system, endocrine system, and immune system all play a role.
If you get migraines, you have a sensitive nervous system. Your body tends to react very quickly, or overreact, to changes in your environment that it views as threats.
On top of that, exposure to allergens triggers your immune system to release certain chemicals. They can fuel inflammation throughout your body, all of which can set you up for a migraine.
If youâre prone to migraine headaches, your symptoms may be more severe during allergy season. Some people can also have ânonallergicâ triggers like perfume, the smell of gasoline, cigarette smoke, and weather changes.
Don’t Miss: Kids Claritin
Treating Allergies Could Help With Migraine
There are certainly scenarios where treating allergies may help headaches, says Strauss. But what we want to avoid is spending years cycling through tons of allergy medicines if someone is having severe headaches. There are other medications wed want to try, she says.
If you have migraine attacks that seem to really be triggered by certain changes in the environment for example, higher pollen or if there is really a lot of nasal congestion or runny nose, then I think it may be worth exploring the role of allergies, says Hamilton.
Strauss suggests keeping a yearly calendar year to see if there are certain months or seasons when migraine attacks become a problem.
This can tip you off if its related to something in the environment, and you could talk with your doctor. It may help to take preventive migraine medications or allergy medicine during those months, she says.
Allergies Could Trigger Migraine Attack In A Few Different Ways
It makes sense that allergies could trigger an attack in people who are predisposed to migraine, says Hamilton. If you’re having a lot of allergic symptoms, and you’re having a lot of inflammation in the body, that could make you more prone to migraine attacks in general, she says.
Some experts believe that the histamine release that happens during allergic reactions can potentially also play a role in migraine, she says. There are potential mechanisms that could explain an increased propensity for migraine when you’re having seasonal allergies, says Hamilton.
Histamine is a chemical found in some cells that can be released when a person is allergic to something, and it causes many of the symptoms of allergies. Histamine release may be involved in triggering a headache, specifically migraine, according an article published in March 2019 in The Journal of Headache and Pain.
Allergies may indirectly contribute to migraine by disrupting sleep, says Strauss. If youre very uncomfortable from all this congestion and postnasal drip, that could even be a trigger for headache, she says.
RELATED: Sleep Tips for People With Migraine
You May Like: Is Coconut Safe For Nut Allergies
Are My Headaches From Allergies
According to the American College of Allergy, Asthma, & Immunology, headaches are among the most common health complaint of Americans, and while some headaches are due to allergies, most are not. There are two types of headaches linked to allergies: sinus, and migraines. It is important to visit your doctor first before ruling out whether or not the particular headache pain you are suffering from is due to an allergy, or another trigger.
So, if the headache is not being triggered by an allergy, then what else could be causing your headache?
If you want to prevent headaches, it is important that you are aware of some of the most common triggers which may lead to a headache. Everyday Health states that you can prevent headaches by avoiding these common causes:
- Stress
- Too much sleep, or not enough sleep
- Excessive exercise
- Eye strain, or sitting at computer
- Caffeine
- Food additives
In order to properly determine what may be causing your headaches, it is important to seek out the opinion of a specialist. A neurologist is a specialist who treats migraines, and is trained in diagnosing and treating disorders of the brain.
To learn more about our providers, and their various specialities visit our Provider Page.
Migraine And Headache Suggestions
1. Keep a headache diary and include your daily intake of these items to help identify a migraine and headache triggers.
- Foods
- Supplements
- Medications
2. Causes of a migraine can overlap with many factors contributing to why you are having increased migraine and/or headaches.
- Learn about your family history with a migraine and headache disorders. If it runs in the family, there is a greater chance that you could inherit a migraine as well.
- Your personal history needs to be looked at carefully to identify any other possible contributors to your headaches/migraine.
Remember that there is help for people who have a migraine with allergies. You can manage them both effectively with the right treatments and modifications.
Underlying allergies can coexist with a migraine, but it does not have to become an untreatable situation.
Related Topics :
You May Like: Cetirizine Hydrochloride Zyrtec
Allergy Headaches: What You Need To Know
Anyone whos ever had an allergy headache knows its terrible. In this guide, we cover facts about allergy headaches you probably DONT knowyet!
Did you know that an estimated 70% to 80% of the population experiences headaches? Whats more, half of these folks who do get headaches deal with such pain at least once a month!
Allergies are also prevalent, affecting at least 50 million people in the US. Theyre so common that theyre now the sixth leading cause of chronic illnesses in the nation.
What a lot of people arent aware of, however, is that allergies can sometimes be the source of the headaches. Either way, an allergy headache can be as bad as or even worse than a typical headache. The symptoms of allergy headaches can even be as intense as those of a migraine.
To that end, weve come up with this guide detailing the link between allergies and headaches. Read on to learn the more about and the things you can do to avoid them.
Can Treating My Allergies Prevent Migraines
So, if you have allergies and migraines, what can you do to feel better?
Well, you can start by treating your allergies. Just like with other migraine triggers, avoiding the trigger in the first place can help you get fewer migraines.
One study found that immunotherapy for allergies helped younger patients get migraines less often.
That said, Dr. Crystal has noticed in her own practice that for some of her patients, starting allergy shots can cause migraines to get worse in the short-term. âPre-treating with an anti-inflammatory prior to the shots may help.â
Read Also: Can Allergies Cause Lymph Node Swelling
Allergies Might Be The Reason For Your Migraine
Allergy season got you down? Flowers are blooming outside, but youre stuck indoors combatting a runny nose. Seasonal allergies and hay fever are quite common, with approximately one in five people in the U.S. experiencing symptoms of these allergies. 1, 2 Such allergies can sometimes be accompanied by headaches and migraines and often, the symptoms are similar. People who have seasonal allergies are more likely to also experience migraine headaches, and many suffer from both conditions at the same time. 2, 3 Additionally, studies have demonstrated that seasonal allergy sufferers are reported to be 4 to 14 times more likely to experience migraine headaches than those without allergies. 4, 5, 6, 7
Both seasonal allergies and migraines may arise due to similar situations such as weather changes or other seasonal migraine triggers. 3 For example, some individuals may be particularly sensitive to ragweed pollen and other fall migraine triggers, while others may be more affected during the spring and summer months, when even the perfume of flowers or other intense smells may trigger migraine headaches. 3
Migraines and seasonal allergies can affect the same parts of the body such as the forehead, the nose and the areas between, behind and around the eyes. 3
One way to help determine if seasonal allergy symptoms actually suggest a migraine headache, or may trigger your headaches, is to keep a migraine diary and share it with your doctor.
References:
What Is The Treatment For Non
Painkillers can help soothe symptoms related to non-sinus related headaches. However, it is best to treat the underlying condition thats causing your headaches to prevent future headaches. For TMJ headaches, a mouthguard worn when sleeping can help prevent headaches. Muscle relaxers may also help prevent muscle-related headaches. Be sure to consult with your doctors before taking any new medication.
Also Check: Difference Between Cetirizine And Levocetirizine
List Of Omicron Variant Symptoms
The variant has the same symptoms of COVID-19, but seems to spread more easily and quickly than other variants, which may lead to more cases of COVID-19, according to the CDC.
People with these symptoms may have COVID-19:
-
Fever or chills
-
Shortness of breath or difficulty breathing
-
Fatigue
-
New loss of taste or smell
-
Sore throat
-
Diarrhea
The Difference Between Symptoms
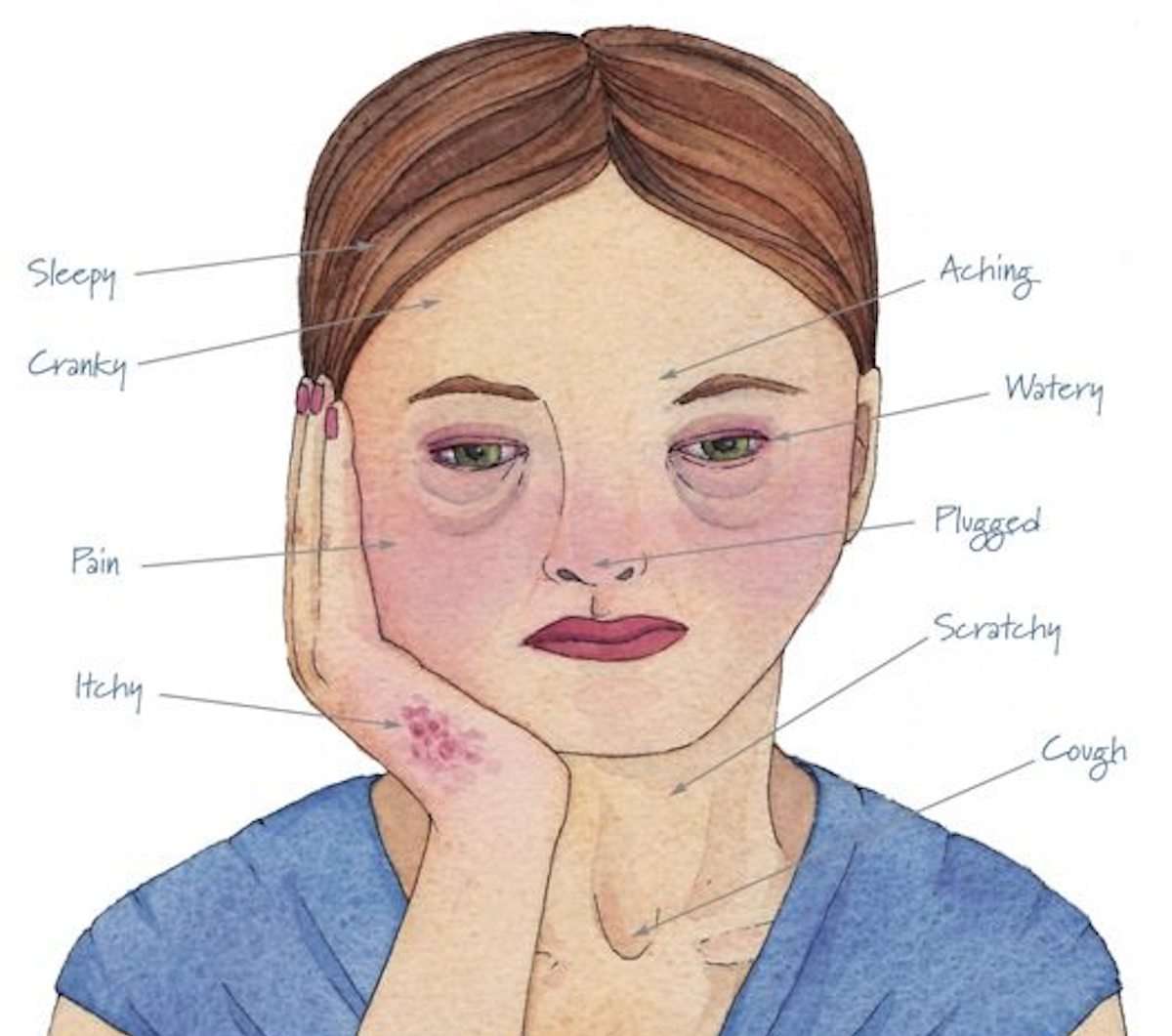
The flu virus and COVID-19 are very similar when it comes to symptoms. Each can come with cough, shortness of breath, fever, headache, chills and a host of other symptoms, but there are some differences, according to the Center for Disease Control and Prevention.
According to the CDC, compared to flu, COVID-19 can cause more serious illnesses in some people. COVID can also take longer before people show symptoms and people can be contagious for longer.
The same goes for allergies and a cold.
The biggest difference could be if someone loses their sense of taste and/or smell.
Because some of the symptoms are similar, it may be hard to tell the difference between them based on symptoms alone, and testing may be needed to help confirm a diagnosis.
Recommended Reading: Can Allergies Affect Lymph Nodes
Allergic Rhinitis And Headaches
Many people do not realise that headaches can be caused by allergic rhinitis but unfortunately it is an uncomfortable and all too common symptom of the condition. Headaches that arise as a result of allergic rhinitis do so for a variety of reasons so, to help make it clearer to you what those reasons are, here our allergy advisor Louise Baillie focuses on the issue in detail.
Louise Baillie
When To See Your Doctor
Although many allergies can be controlled with judicial use of OTC medications, its always wise to consult with your doctor. If allergies are negatively impacting your quality of life or interfering with your daily activities, its in your best interests to explore treatment options with your doctor.
Your doctor might recommend that you see an allergist. This is a physician specializing in diagnosing and treating allergic conditions, such as asthma and eczema. An allergist might offer you a number of suggestions for treatment, including:
Don’t Miss: Keflex Amoxicillin Allergy
How Can I Tell The Difference Between Earlier Strains Of Covid And The New Omicron Variant
The new omicron variant has double the mutations of the delta variant and there are now cases of it worldwide.
Key symptoms include fatigue and a high pulse rate but do not include those associated with the earlier strains, such as a fever or loss of taste or smell.
The omicron variant differs to earlier strains and is more easily distinguished against the common cold. Those who contract the common delta variant of Covid tend to display symptoms of coughing, a runny nose, a sore throat and headaches – which are associated with the common cold.
Get Help With Your Allergy Headaches
Combining an antihistamine with an analgesic will offer fast relief for your allergy attacks and headaches. Over-the-counter antihistamines include Benadryl, Zyrtec and Claritin commonly available analgesics include Advil and Aleve. NSAIDS such as Advil and Aleve are the most effective in stopping allergy headache pain, but if you cannot take those, Tylenol may be your best option. Its important to remember that any antihistamine, especially Benadryl can cause drowsiness and you should avoid driving or any other dangerous activity after taking it. But those are just short-term solutions for a longer-term issue.
If you suffer from severe allergy headaches and want lasting treatment for them, we can help. Live the pain-free life you deserve! Contact us today for a consultation via telemedicine or in-person.
You May Like: Does Claritin Help With Itchy Skin
The Link Between Migraine And Allergies
Additional research showed that migraine occurred 14 to 28 percent more frequently in those with migraine and allergies than in those with migraine alone. Allergies and asthma also cause people with episodic migraine to be more than twice as likely to develop chronic migraine . Another study showed that there is an increased risk of migraine in children with asthma.
So Can Allergies Give You A Headache
For the record, yes, allergies can cause a headache, says Anastasiya Kleva, MD, a board-certified allergist at ENT and Allergy Associates NY. They can cause a lot of pain, particularly around the sinuses, she says.
How? You inhale allergens, which cause inflammation in your nose, explains Lakiea Wright, MD, an allergist/immunologist at Brigham and Womens Hospital in Boston and the medical director at Thermo Fisher Scientific. If your nose is congested, the inflammation can also spread to your sinuses. When inflammation accumulates in your sinuses, then you can get a headache.
Allergies can also cause your ears to get clogged, and that can lead to a headache, says Purvi Parikh, MD, an allergist and immunologist with the Allergy & Asthma Network.
Don’t Miss: Difference Between Fexofenadine And Loratadine
Are Allergies Triggering Your Migraine Attacks
While allergies can trigger migraine attacks, its also possible that you just have both conditions simultaneously.
Adobe Stock
For some people with allergies, symptoms like sneezing, sinus congestion, and watery eyes can also come with a headache. Many people who experience head pain with their allergies wrongly assume its just another symptom of allergies, or a sinus headache, according to Lauren Doyle Strauss, DO, a headache specialist and an assistant professor at Wake Forest Baptist Health in Winston Salem, North Carolina.
I see people with allergies who think they have sinus headaches when in reality, many of them meet the criteria for migraine, says Dr. Strauss.
If youre living with both conditions, the one-two punch of allergies and migraine can keep you indoors and away from friends and activities for weeks or even months, depending on the season. Find out how allergies may be triggering or worsening migraine and what the experts advise about seeking diagnosis and treatment.
RELATED: Is It a Migraine Attack or a Sinus Headache?
How Long To Quarantine After Positive Covid Test
The Centers for Disease Control and Prevention on Monday cut the amount of time it recommends people should isolate after testing positive for COVID-19, reducing the number of days from 10 to five.
Health officials similarly reduced the amount of time one should quarantine after coming into contact with someone who tests positive.
The changes come amid a recent surge in cases spurred by the omicron variant and concerns about staffing shortages at hospitals, airlines and businesses across the country. Research has suggested omicron, while more infectious, causes milder illness. CDC officials say the new guidance is in keeping with growing evidence that people with the coronavirus are most infectious in the two days before and three days after symptoms develop.
More: CDC cuts isolation time for Americans who test positive for COVID-19 from 10 days to 5: Updates
Also Check: Clairitn

