Ige Mediated Food Allergies
The IgE mediated food allergies most common in infants and children are eggs, milk, peanuts, tree nuts, soy and wheat. The allergic reaction can involve the skin, mouth, eyes, lungs, heart, gut and brain. Some of the symptoms can include:
- Skin rash, itching, hives
- Swelling of the lips, tongue or throat
- Shortness of breath, trouble breathing, wheezing
- Stomach pain, vomiting, diarrhea
- Feeling like something awful is about to happen
Sometimes allergy symptoms are mild. Other times they can be severe. Take all allergic symptoms seriously. Mild and severe symptoms can lead to a serious allergic reaction called anaphylaxis . This reaction usually involves more than one part of the body and can get worse fast. Anaphylaxis must be treated right away to provide the best chance for improvement and prevent serious, potentially life-threatening complications.
Treat anaphylaxis with epinephrine. This medicine is safe and comes in an easy-to-use device called an auto-injector. You cant rely on antihistamines to treat anaphylaxis. The symptoms of an anaphylactic reaction occur shortly after contact with an allergen. In some individuals, there may be a delay of two to three hours before symptoms first appear.
Cross-Reactivity and Oral Allergy Syndrome
Cross-reactivity also can occur between latex and certain foods. For example, a child who has an allergy to latex may also have an allergy to bananas, avocados, kiwis or chestnuts.
Non Lge Mediated Symptoms
For milk allergy, non-IgE-mediated responses are more common than IgE-mediated. The presence of certain symptoms, such as angioedema or atopic eczema, is more likely related to IgE-mediated allergies, whereas non-IgE-mediated reactions manifest as gastrointestinal symptoms, without skin or respiratory symptoms. Within non-IgE cow’s milk allergy, clinicians distinguish among food protein-induced enterocolitis syndrome , food protein-induced allergic proctocolitis and food protein-induced enteropathy . Common trigger foods for all are cow’s milk and soy foods . FPIAP is considered to be at the milder end of the spectrum and is characterized by intermittent bloody stools. FPE is identified by chronic diarrhea which will resolve when the offending food is removed from the infant’s diet. FPIES can be severe, characterized by persistent vomiting, 1 to 4 hours after an allergen-containing food is ingested, to the point of lethargy. Watery and sometimes bloody diarrhea can develop 5 to 10 hours after the triggering meal, to the point of dehydration and low blood pressure. Infants reacting to cow’s milk may also react to soy formula, and vice versa. International consensus guidelines have been established for the diagnosis and treatment of FPIES.
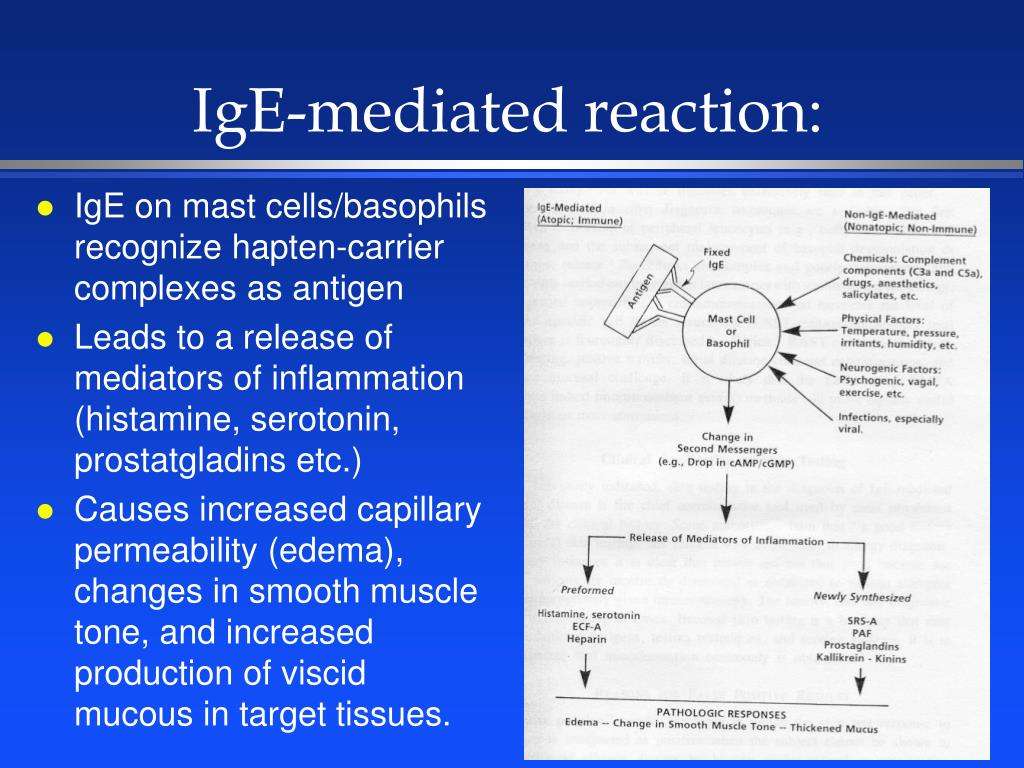
Amplification Of The Ige Response To Allergens Through Fcri
IgE does not fix complement and has only limited ability to cross the placenta, and it is thought that IgEâs main biological roles reflect its ability to bind to receptors on mast cells, basophils and a variety of other cell types. The high-affinity receptor for IgE, FcεRI, as expressed by mast cells and basophils, consists of an IgE-binding α chain, in which the two extracellular domains bind IgE, a β chain, which spans the plasma membrane four times and functions as a signal amplifier, and two identical and largely intracellular γ chains. The signaling motifs of this αβγγ form of FcεRI consist of immunoreceptor tyrosine-based activation motifs, one in the β chain and one in each of the γ chains. An αγγ form of the receptor can be expressed on a variety of other cell types, including macrophages, dendritic cells, eosinophils, platelets and neutrophilsâ .
Don’t Miss: Kit Kats Peanut Allergy
Listen To Our Allergy And Immunology Pediatric Expert Discuss Non
On today’s episode, we welcome back Matthew Greenhawt, MD, to discuss non-IgE related food allergies, including Food Protein-Induced Enterocolitis Syndrome . FPIES is a rare non-IgE mediated food allergy with delayed onset symptoms that can be difficult to identify, but PCPs who understand the symptoms and triggers can help kids get help sooner.
Dr. Greenhawt is Director of the Food Challenge and Research Unit at Children’s Hospital Colorado and an associate professor of pediatrics and allergy at the University of Colorado School of Medicine.
Alternative Tests For Food Allergy
Some complementary or alternative health practitioners offer tests for food allergy. These can include tests called applied kinesiology, hair analysis, vega tests and serum-specific IgG antibody tests. Your healthcare professional should not offer your child these tests because there is no evidence that they can reliably diagnose food allergy.
Read Also: Zyrtec Hives Relief Tablets
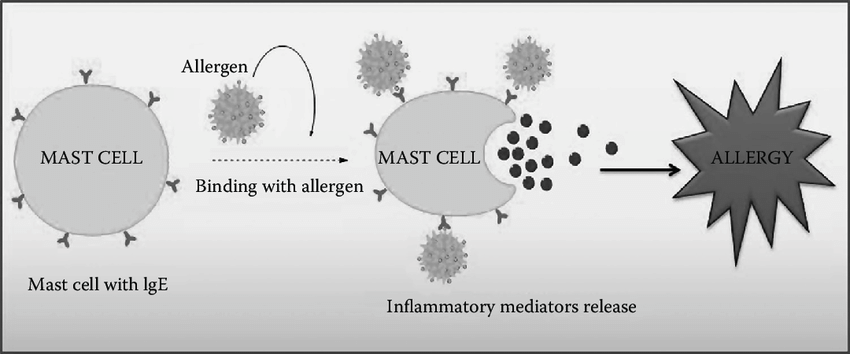
The Role Of Ige In Allergic Inflammation
Sensitization
The immune response in allergy begins with sensitization. When, for example, house dust mite or pollen allergens are inhaled, antigen presenting cells in the epithelium lining of the airways of the lungs and nose, internalise, process and then express these allergens on their cell surface. The allergens are then presented to other cells involved in the immune response, particularly T-lymphocytes. Through a series of specific cell interactions B-lymphocytes are transformed into antibody secretory cells – plasma cells. In the allergic response, the plasma cell produces IgE-antibodies, which, like antibodies of other immunoglobulin isotypes, are capable of binding a specific allergen via its Fab portion. Different allergens stimulate the production of corresponding allergen-specific IgE antibodies. Once formed and released into the circulation, IgE binds, through its Fc portion, to high affinity receptors on mast cells, leaving its allergen specific receptor site available for future interaction with allergen. Other cells known to express high-affinity receptors for IgE include basophils, Langerhans cells and activated monocytes. Production of allergen specific IgE-antibodies completes the immune response known as sensitization.
Re-exposure to allergen
Early and late phase reactions
To see a video of the IgE-mediated allergic response .
IgE and the nomenclature of allergic disease
Amplification Of The Ige Response To Allergens Through Cd23
Once an individual has developed IgE antibodies to certain antigen epitopes, multiple mechanisms can lead to a more robust and diverse IgE responses to both the original as well as other antigens. Some of these mechanisms are mediated by CD23 , which can be expressed on cells such as epithelial cells, B cells and myeloid cells . CD23 is a C-type lectin that can exist in a membrane-bound form that has three lectin domain âheadsâ separated from the membrane by a triple α-helix coiled-coil stalk, as well as in various soluble forms whose functions depend on whether these soluble forms are monomeric or trimeric, . The CD23 sheddase, ADAM metallopeptidase domain 10 , is the main protease that releases soluble CD23 from the membrane-associated form,. CD23 is sometimes called a low-affinity receptor for IgE, but when the three lectin head domains of CD23 interact with a single IgE molecule, the resulting affinity constant approaches that of the high-affinity receptor for IgE, Fcε receptor I ,.
Don’t Miss: Can Allergies Cause Swollen Tonsils
Youll Understand Your Body Better
If you decide to have proper IgE allergy testing, youllunderstand how your body reacts to the food that you are eating, and howavoiding these key ingredients will make you healthier in the long-term. Having a food allergy is serious andimportant to know, but once you get the rest results back, you can back incontrol of your own body and be able to improve your overall quality of life asa result.
Why We Need To Stop Referring To Ige
The way we currently talk about food allergies minimizes the visibility of non-IgE food allergies, and the impact they have on families.
Guest post by Mun Cho, registered dietitian
Originally published in The Mighty and reposted by The FPIES Foundation, this guest blog post by registered dietitian Mun Cho shares the experience of managing non-IgE-mediated food allergies, conditions that can be unfamiliar to healthcare providers. To learn more about non-IgE-mediated food allergies, register for next week’s FARE webinar, , presented by Dr. David Stukus on Monday, May 17, at 12:00 p.m. ET.
This is an open letter to all healthcare professionals from a food allergy mama and Registered Dietitian.
I am writing to you as a mother to children with both IgE-mediated and non-IgE-mediated food allergies. As many of you are aware, allergic reactions commonly seen in the media are IgE reactions those that could turn into fatal anaphylaxis. The less commonly talked about food allergies are non-IgE reactions, such as food protein-induced enterocolitis or a non-IgE cows milk protein allergy. These ones are non-anaphylactic, and come with mostly gut-related symptoms. But they are still real allergies.
When we label IgE food allergies as true food allergies, it leaves little space for other forms of food allergies to be taken seriously. We need to go beyond the conversation that true food allergies lead to anaphylaxis. And we need to change the language we use.
You May Like: Dextromethorphan Is An Antihistamine Used To Dry Up A Runny Nose.
How Do You Know If Your Immune System Is Compromised
The American Academy of Allergy Asthma & Immunology reports that signs of a possible immune deficiency in adults include: Having more than four ear infections in one year. Developing pneumonia twice during a one-year period. Suffering from chronic sinusitis or more than three episodes of bacterial sinusitis in a year.
Signs And Symptoms Of Ige
When your child has a food allergy, her bodys IgE antibodies identify that specific food as an invader and can produce symptoms in multiple areas of the body, including:
- Skin: hives , mild to severe swelling
- Eyes: tearing, redness, itch
- Nose: clear discharge, itch, congestion
- Mouth: itch, lip swelling, tongue swelling
- Throat: tightness, trouble speaking, trouble inhaling
- Lungs: shortness of breath, rapid breathing, cough, wheeze
- Stomach: repeated vomiting, nausea, abdominal pain, diarrhea
- Heart and circulation: weak pulse, loss of consciousness
- Brain: anxiety, agitation, loss of consciousness
Allergic reactions can be scary, but noticing symptoms early can help your child get proper treatment.
Reactions to food can be different every time. Your childs reaction can depend on a variety of factors including the amount of food eaten, uncontrolled asthma, and illness. In addition, the way the food was prepared and the amount of food protein ingested can affect your childs reaction.
Read Also: Dextromethorphan Allergic Reaction
How Are Ige Levels Reported
The total IgE reference range depends on the age of the individual .
The result of a specific IgE test is reported for a grouped allergen mix or an individual allergen. The table below shows how the results are typically rated and interpreted .
Table. IgE level test ratings and interpretations
| Rating of specific IgE level | Grade/Class |
|---|---|
| VI | Extremely likely |
This table shows arbitrary international reference figures. The actual reference range and grading vary with the laboratory and are based on the method used for the test, calibration, the age of the patient, and the type of allergens.
Box 2 Late Phase Reactions And Chronic Antigen Exposure Lead To Persistent Allergic Inflammation And Tissue Remodeling
In addition to possible redundancy in the roles of mast cells and other cell types in the chronic changes associated with asthma, there is evidence that many factors can modify mast cell function in this setting. For example, in vitro,â and in vivo,, evidence indicates that the extent of antigen- and IgE-dependent mast cell activation may be influenced substantially by microenvironmental factors that affect the expression or function of surface receptors or signaling molecules that contribute to the positive or negative regulation of such responses,,,,. Tuning factors that can be present locally at the sites of allergic inflammation, such as in the airways and other anatomical sites, include adenosine, sphingosine-1 phosphate , certain chemokines and a variety of cytokines, such as IL-4 , IL-33 and interferon γ . Tuning also can be accomplished by cell-cell interactions. For example, interactions of mast cells and T cells can be bidirectional and complex, and include the ability of IgE-activated mast cells to enhance proliferation and cytokine production in multiple T cell subsets, and the ability of CD4+CD25+ regulatory T cells to suppress IgE-dependent mast cell activation through interactions between tumor necrosis factor receptor superfamily, member 4 , either as expressed by Treg cells or in a soluble form, and the OX40 ligand, OX40L expressed on mast cells .
Also Check: Zyrtec Dissolvable Tablets
What Foods Increase Ige
Specific IgE levels were highest for peanuts, followed by cows milk, eggs, soy, and almonds, and trended upward over time. Conclusion: In children presenting with clinical symptoms of a reaction to a food allergen, measurements of food-specific serum IgE to other common food allergens are commonly positive.
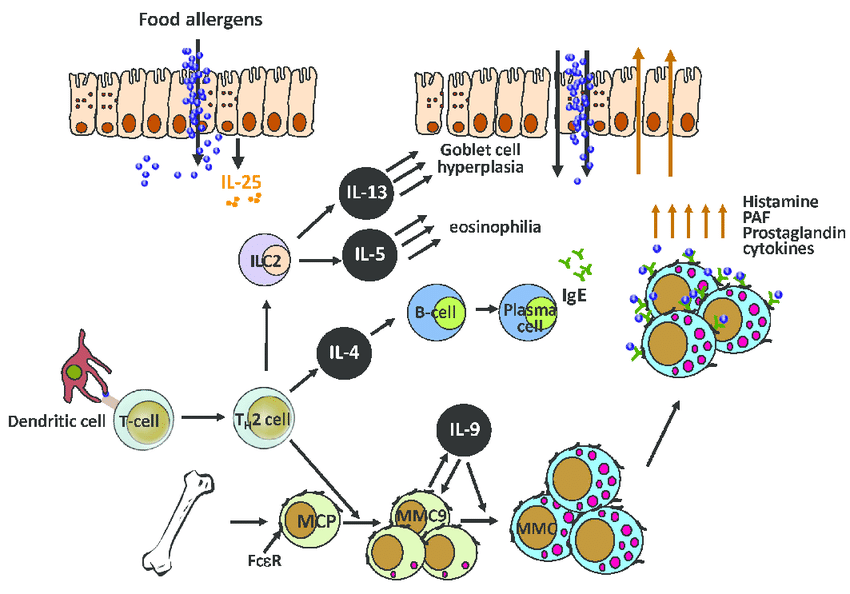
Antigen Presenting Cells And Innate Lymphoid Cells
In the absence of sensitizing chemical mediators, CX3CR1+ macrophages can sample antigen and produce the cytokine IL-10, which will allow for the differentiation of naïve T cells to regulatory T cells. CD103+ dendritic cells can also capture antigen directly or from transfer by the macrophage . CD103+ DCs will migrate to draining lymph nodes and present the antigenic peptide along with the class 2 major histocompatibility complex to naïve T cells. Furthermore, in the presence of TGF- and retinoic acid secreted from the DCs, naïve T cells are promoted toward a tolerant phenotype and can differentiate to T regulatory cells .
Conversely, the breakdown of tolerance due to a compromised epithelial barrier, promotes the epithelial release of pro-inflammatory chemical mediators, such as IL-25, IL-33, and TSLP . These mediators act upon antigen presenting cells and innate lymphoid cells, to further promote sensitization by a Th2 phenotype. Activated dendritic cells promoting allergy, express surface OX40L, also known as tumor necrosis factor ligand superfamily member 4 and migrate to the draining lymph node where they encounter and present antigen to naïve T cells . The MHC of the dendritic cell presents antigenic food peptides to naïve T cells and with the interaction between OX40L on DCs and OX40 on naïve T cells, differentiation occurs from naïve T cells into Th2 T cells, thus promoting the allergic state.
Recommended Reading: Twix Peanuts
Toxin Hypothesis Of Allergic Disease
In 1981 suggested that allergic reactions have evolved as a last line of defense to protect against venoms. Although controversial at the time, new work supports some of Profets thoughts on the adaptive role of allergies as a defense against noxious toxins.
In 2013 it emerged that IgE-antibodies play an essential role in acquired resistance to honey bee and Russell’s viper venoms. The authors concluded that “a small dose of bee venom conferred immunity to a much larger, fatal dose” and “this kind of venom-specific, IgE-associated, adaptive immune response developed, at least in evolutionary terms, to protect the host against potentially toxic amounts of venom, such as would happen if the animal encountered a whole nest of bees, or in the event of a snakebite”. The major allergen of bee venom induces a Th2 immune responses, associated with production of IgE antibodies, which may “increase the resistance of mice to challenge with potentially lethal doses”.
Testingskin Testing And Serum
In addition to the detailed medical history and physical examination, when suspecting an IgE-mediated food allergy, the practitioner can utilize clinically approved tests, to aid in the diagnostic workup. Commonly utilized tests such as the immediate hypersensitivity skin test and food-specific IgE antibody tests are utilized in the evaluation of an IgE-mediated food allergy. It is important for general practitioners and allergists to be aware of the dangers of ordering large panels of tests which can lead to false-positive results and potentially unnecessary dietary eliminations. In addition, a 46-week waiting period after an anaphylaxis episode should be given before skin testing is performed.
Table 4 Diagnostic cut-offs for immediate hypersensitivity skin-prick testing and serum food-specific IgE testing , negative predictive value )
You May Like: Allergic Reaction To Claritin
Living With Dietary Restrictions
Regardless of the allergic condition, the affected person must avoid consuming the food that triggers the allergic reaction. Even trace amounts of the allergen can provoke symptoms, so strict avoidance is recommended.
Living with dietary restrictions can be very challenging, considering the prevalence of processed and prepared foods which often contain a long list of ingredients. The allergic individual should read all nutrition labels carefully in order to identify the presence of an allergen. In addition, products labelled as may contain, should be avoided.
Allergic individuals should also avoid cross-contact between foods. This is when an allergen is inadvertently transferred from one food to another, by way of a contaminated surface. Examples of risk for cross contact can include sharing contaminated surfaces . Several precautions must be taken when purchasing and preparing meals for allergic individuals.
SUGGESTED READING:
Sensitization To Foods By The Oral Route
Although there is compelling evidence that sensitization to peanut may occur through skin exposure, there is also likely contribution of the mucosal immune system in food allergy. Cow’s milk is most often the earliest food introduced into the diet, and milk allergy is the most common allergy of early childhood. Eigenmann et al. demonstrated that T cells from milk-allergic donors stimulated with milk antigen in vitro upregulated the gut-homing marker 47, which was not seen with the control antigen tetanus or in milk-tolerant controls. This is suggestive of gastrointestinal immune priming to milk. Therefore, it is likely that sensitization may occur in the gastrointestinal tract to some foods. Further evidence supporting an oral route of sensitization comes from the finding that antacid treatment of mice and humans increases the level of sensitization to food antigens , .
You May Like: Clearitin
How Does Ige Testing Compare With Skin Prick Testing
Skin prick testing is more specific than IgE testing and gives a rapid result , but it requires a trained practitioner and is not always tolerated by young children.
Specific IgE blood tests are simple and safe. They can be expensive, depending on the number of allergens tested. Caution is required when interpreting the results .
What Is An Ige Mediated Reaction
5/5IgEmediatedreactreactionsin-depth answer
IgE–mediated means that IgE allergy antibodies are a cause of the allergic reaction to a food. By contrast the signs and symptoms of IgE mediated food allergy usually occur within minutes of ingestion and include hives, redness of the skin, vomiting and in more severe reactions, anaphylaxis.
Furthermore, what are the 4 types of allergic reactions?
- Type I: Immediate Hypersensitivity These allergic reactions are systemic or localized, as in allergic dermatitis .
- Type II: Cytotoxic Reaction
- Type III: Immune Complex Reaction.
- Type IV: Cell-Mediated
Thereof, what is the difference between IgE and non IgE reactions?
IgE-mediated reactions typically occur immediately after ingestion whereas non–IgE mediated are delayed and take up to 48 hours to develop, but still involve the immune system.
Are all allergies IgE mediated?
Underlying Mechanisms of Food AllergyTypical food allergies are IgE–mediated, but several reactions involve different immunologic mechanisms. These food allergies are defined as nonIgE–mediated or mixed IgE– and nonIgE–mediated.
Recommended Reading: Are There Nuts In Twix

