Cdc Is Monitoring Reports Of Severe Allergic Reactions
If someone has a severe allergic reaction after getting vaccinated, their vaccination provider will send a report to the Vaccine Adverse Event Reporting System .external icon VAERS is a national system that collects reports from healthcare professionals, vaccine manufacturers, and the public about adverse events that happen after vaccination. Reports of adverse events that are unexpected, appear to happen more often than expected, or have unusual patterns are followed up with specific studies.
Information From The Cdc On The Covid
The Centers for Disease Control and Prevention released guidelines for the current COVID-19 vaccines. The Pfizer-BioNTech and Moderna COVID-19 vaccines were the first to be authorized by the FDA. The Pfizer-BioNTech is the first to be approved. They are mRNA-type vaccines. The mRNA vaccines teach your immune system to make a protein that starts an immune process. Your body then produces antibodies that can protect you from COVID-19.
The Pfizer-BioNTech vaccine is a shot given in two doses three weeks apart. The Moderna vaccine is also given in two doses about four weeks apart. Based on the clinical trials, you need both doses of these to be fully protected from COVID-19. If you are immunocompromised, it is recommended you get a third dose at least 28 days after your second shot.
The Johnson & Johnson vaccine is only given in one shot. There is no recommendation for an additional or booster dose for the J& J COVID-19 vaccine at this time. It is a viral vector vaccine. It is different than mRNA vaccines. A viral vector vaccine uses a modified version of a different virus to deliver instructions to cells in your body. This triggers your body to create antibodies to SARS-CoV2, the virus that causes COVID-19. You cannot get COVID-19 from this vaccine since it is a modified virus.
None of the vaccines will affect your DNA. These vaccines reduce the chance of getting COVID-19. They can also reduce the severity of your symptoms if you get the disease.
Mhra Statement On Guidance To Vaccination Centres On Managing Allergic Reactions Following Covid
Dr June Raine, Chief Executive of the Medicines and Healthcare products Regulatory Agency , said:
We have this evening issued updated guidance to COVID-19 vaccination centres about the management of anaphylaxis, following two reports of anaphylaxis and one report of a possible allergic reaction following immunisation. This guidance confirms the precautionary advice to healthcare professionals which we issued yesterday evening.
Today we convened an Expert Group of the Commission on Human Medicines , attended by experts in allergy and clinical immunology, to robustly review these reports to consider any possible mitigation on the rare risk of anaphylaxis.
Also Check: Robitussin Nasal Congestion
Who Can Get The Covid
People 12 and older can get the Pfizer-BioNTech COVID-19 vaccine. People 18 or older can get the Moderna or J& J COVID-19 vaccines. You can get your shot at a local pharmacy, clinic, or vaccination center. Go to vaccines.gov to find a location. The vaccine is free to everyone.
Do not take over-the-counter pain medicines like acetaminophen or ibuprofen before getting a COVID-19 vaccine to reduce side effects. Taking the over-the-counter pain medicines or anti-inflammatories may stop the vaccine from working as it should and reduce its ability to make antibodies. Talk with your doctor about taking pain medicines after you get the shot.
If you get another type of vaccine , make sure you wait 14 days before getting the COVID-19 vaccine.
If you get allergy shots , talk with your allergist if your shot schedule overlaps with getting the COVID-19 shot. There are no data on allergy shots and the COVID-19 vaccine at this time. But to help reduce confusion if you have local reactions or side effects, it may help to spread these out by a couple days.
The following people can get a COVID-19 vaccine:
Your doctor may need to give you more information about the vaccine depending on your condition.
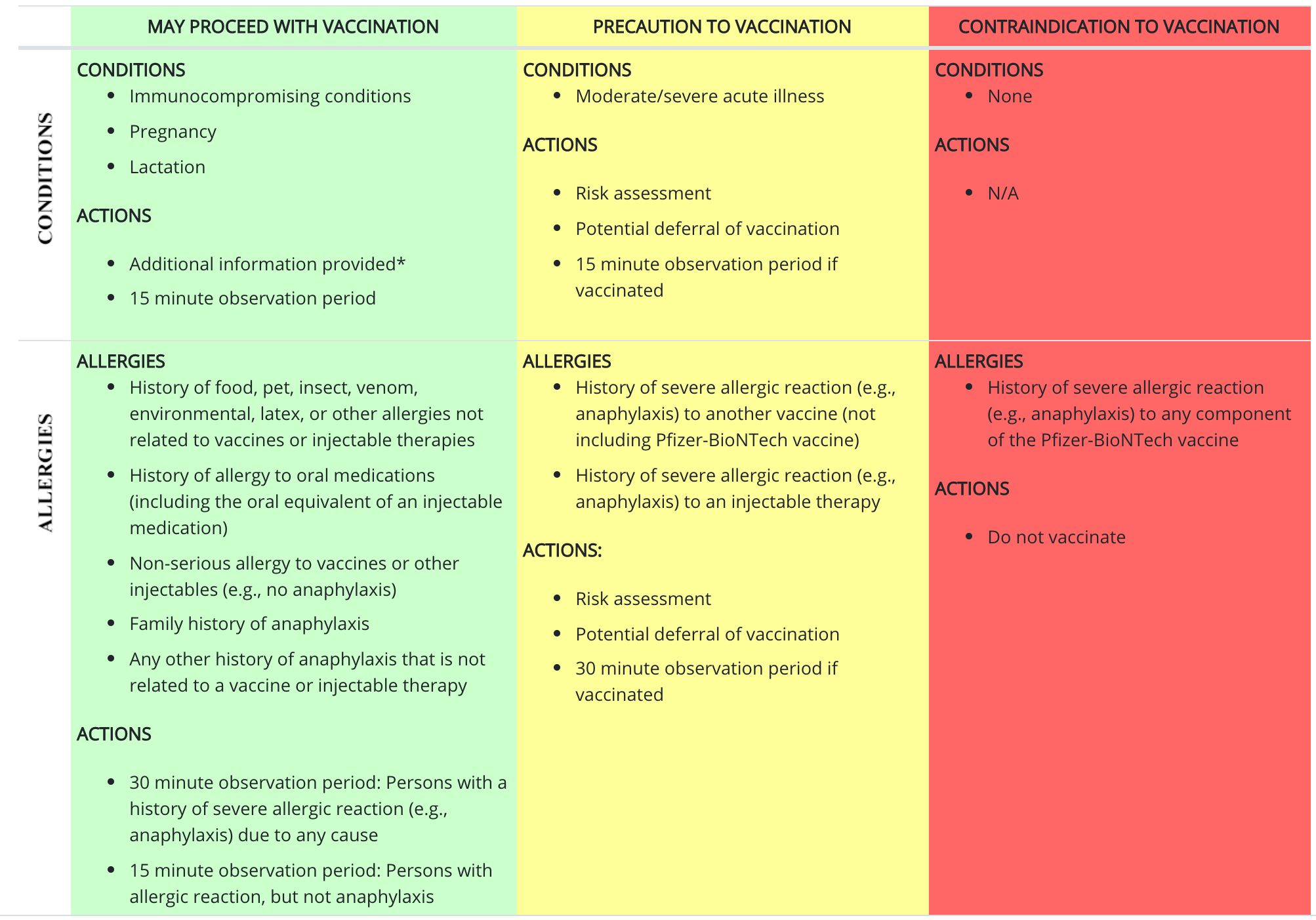
If you have a history of severe allergic reactions , you may be monitored up to 30 minutes after the shot. For everyone else, you will be monitored for 15 minutes after the shot.
If you have a reaction to the first dose of an mRNA vaccine , talk with your doctor about your options.
Should You Take Otc Medications Before Getting The Vaccine

Taking OTC pain medications ahead of your shot to try and decrease symptoms is not recommended by the CDC, because it’s not clear how that could affect the vaccine’s effectiveness.
The concern is that pre-treating with pain medications that reduce fevers and inflammation could dampen your immune system’s response to the vaccine.
That’s because your immune system responds to vaccines through a process called “controlled inflammation,” Dr. Colleen Kelley, an associate professor of medicine at Emory University School of Medicine, told USA Today in January.
Covid messenger RNA vaccines work by giving cells genetic material that tells them how to make a non-infectious piece of the virus. The immune system then creates antibodies against it which is controlled inflammation and can remember how to trigger an immune response if exposed to the virus in the future.
But OTC pain-relieving medications “reduce the production of inflammatory mediators,” Kelley said. That’s why it’s important to wait until after you’ve gotten the vaccine to take pain medication.
Research on children has shown that those who take acetaminophen before getting vaccines have a lower immune response than those who didn’t. And a recent study out of Yale found that giving mice nonsteroidal anti-inflammatory drugs before being exposed to SARS-CoV-2 led to fewer protective antibodies from the virus.
You May Like: Is Mucinex Good For Allergies
If You Get A Rash Where You Got The Shot
CDC has learned of reports that some people have experienced a red, itchy, swollen, or painful rash where they got the shot. These rashes can start a few days to more than a week after the first shot and are sometimes quite large. These rashes are also known as COVID arm. If you experience COVID arm after getting the first shot, you should still get the second shot at the recommended interval if the vaccine you got needs a second shot. Tell your vaccination provider that you experienced a rash or COVID arm after the first shot. Your vaccination provider may recommend that you get the second shot in the opposite arm.
If the rash is itchy, you can take an antihistamine. If it is painful, you can take a pain medication like acetaminophen or a non-steroidal anti-inflammatory drug .
Vaccine Team: Can I Take Pain Relievers Or Allergy Medicine After My Covid
When you can and should not take medicines
CHARLOTTE, N.C. – As more people across the Carolinas are up for their second dose of the COVID-19 vaccine, were answering your questions.
Robin reached out to the Vaccine Team before her second dose: Can I take pain relievers or allergy medicine after my COVID-19 vaccine?
Please read this carefully.
Yes, AFTER your shot, you can treat any aches with simple pain relievers, according to the Centers for Disease Control and Prevention.
However, the CDC says you should not take pain relievers BEFORE your shot.
It is not recommended you take over-the-counter medicine such as ibuprofen, aspirin, or acetaminophen before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works. However, if you take these medications regularly for other reasons, you should keep taking them before you get vaccinated. It is also not recommended to take antihistamines before getting a COVID-19 vaccine to try to prevent allergic reactions.
Some other ways to prevent feeling badly after your shot is to make sure you are well-rested, hydrated, and make sure you dont have an empty stomach.
Other recommendations to help with soreness at the site of injection put a cool cloth on the injection site, move your arm around after your shot.
If you have a question for the WBTV Vaccine Team, submit your question here.
Most Read
Also Check: Is Pine Nuts A Nut Allergy
Is Taking Medicines After The Covid
As per Dr. DN Jha, Senior Consultant- MBBS, MD, Internal Medicine at Batra Hospital, New Delhi, regular medicines for comorbidities and coronavirus vaccine shot, both are equally important for your health and body. You cannot miss out on the regular medicine dose to manage the existing condition and covid-19 vaccination is a must to protect oneself from the deathly virus attack. No one has cared if both can be merged or if there any side-effect when these drugs meet in the body. It is very important to know this to potentially ward off the unforeseen casualty that may arise in the future.
Besides, people with comorbidities have a compromised immune system that increases the risk of infection in them. This is why they need to get vaccinated but if they are taking medications, it is better to speak to a doctor before taking the jab. Coronavirus is an autoimmune disease and its vaccine is made to generate an autoimmune response to fight the virus if it enters the body. However, vaccination may act slower in their bodies due to poor immunity and this can cause a delayed vaccine response. But vaccination is a must to keep safe from this infection.
The Mhra Has Issued Specific Guidance Over Who Should Not Get The Vaccine
Wondering if you need to skip the COVID vaccine? Per Reuters, the MHRA sent out new guidance to healthcare professionals that advised, “Any person with a history of a significant allergic reaction to a vaccine, medicine or food should not receive the Pfizer BioNtech vaccine.” And for more on the coronavirus vaccine, This Is What Happens If You Only Get One Dose of the COVID Vaccine.
You May Like: Does Twix Contain Peanuts
Allergy Asthma Medication Could Help Against Covid
VIRGINIA BEACH, Va. – There is no vaccine right now to cure COVID-19, and researchers are racing to develop one. However, if you have allergies or asthma, your medication could help you against the virus, according to Dr. Angela Hogan, an allergist and immunologist at The Childrens Hospital of the Kings Daughters.
Being allergic sort of turns on different immune cells in the body, Hogan explained. What we know in patients who have asthma is that the same sorts of things that drive asthma turn off certain immune cells.”
These immune cells, Hogan said, are cells the COVID-19 virus targets to infect in order to spread.
In fact, the proportion of patients who have asthma that are getting significant respiratory impact from the COVID-19 is much lower than what was predicted,” Hogan said.
Hogan said certain additives in these medications, such as enhanced steroids, are what helps. Some medications she mentioned included Flovent, Qvar, Advair and Symbicort.
If someone were to purchase allergy or asthma medications and consume them despite not suffering from those conditions, Hogan said these medications would have no effect.
I think that its important to be on your medications, especially your asthma medications, so that your asthma is well-controlled in the event you get the COVID-19 infection,” Hogan said.
Hogan said this season in particular was worse for allergy sufferers due to abnormal weather conditions.
Dr Fauci Said Do Expect Some Side Effects Especially After The Second Dose
âIf you are really having discomfort that usually would occur rarely after the first dose, you likely would get a pain in the arm and maybe a little bit of an ache, not very much of an issue there. Thatâs what I went through personally, when I got it,â he said. âBut the second dose of either the Madonna or the Pfizer in some people do get about a 24 hours worth of achiness, maybe some chills, occasionally a fever, a headache. You feel under the weather, as it were taking something appealed to youlike two Tylenol, every six or eight hours or soI can see is going to have a major difference that might make you feel much better.â
Recommended Reading: Can A Gluten Allergy Cause A Rash
Preparing For Your Covid
NOTICE: FDA has granted full approval for Pfizer-BioNTech COVID-19 Vaccine. CDCs Advisory Committee on Immunization Practices is meeting on Monday, August 30, 2021, to discuss its updated recommendation for this vaccine.
COVID-19 vaccines are effective at protecting you from getting sick even after you have had COVID-19. Vaccination is an important tool to help us get back to normal. This information will help you prepare for your COVID-19 vaccination.
Learn more about the different types of COVID-19 vaccines and how they work.
Find a COVID-19 Vaccine: Search vaccines.gov, text your ZIP code to 438829, or call 1-800-232-0233 to find locations near you.
What To Do After Covid
When Bharat Biotech’s Covaxin was allowed for restricted emergency use under the clinical trial mode in January, beneficiaries had to fill a form mentioning whether they had any kind of allergies as the company at that time suggested advised not to take the vaccine if one has allergies. As Bharat Biotech provided more data, its vaccine was removed from the ‘clinical trial’ mode.
So, can people with allergies can take Covaxin now? Without specifying the name of the vaccine, Dr VK Paul of Niti Aayog said if one has a severe allergy issue, then it’s better to consult a doctor before getting vaccinated. But if it is a common allergy issue of skin, then there should be no hesitation to take any Covid-19 vaccines.
-19 #Unite2FightCorona#StayHomeStaySafe
#IndiaFightsCorona
AIIMS director Dr Randeep Guleria said if one is on allergy medication, then the medication should be continued after vaccination. “If there is any allergic reaction post the vaccination, then once can report to the doctors at the vaccination centre,” Dr Guleria said.
According to Bharat Biotech, the manufacturer of the vaccines, individuals with a history of allergies to oral medications or a family history of allergic reactions, or who might have a mild allergy to vaccines may still get vaccinated.
Read Also: Is Pine Nuts A Nut Allergy
When Can I Get My Allergy Shot After Receiving The Vaccine
If you are undergoing immunotherapy for your allergies, we recommend the COVID-19 vaccine and the allergy shot be administered at least 24-48 hours apart. While we have not seen any reasons for patients on allergy shots not to receive either the mRNA COVID-19 vaccines or the Johnson & Johnson vaccine, waiting 24-48 hours helps avoid confusion if a reaction occurs.
Treating Severe Allergic Reactions
Some people with severe allergies may experience life-threatening reactions, known as anaphylaxis or anaphylactic shock.
If you’re at risk of this, you’ll be given special injectors containing a medicine called adrenaline to use in an emergency.
If you develop symptoms of anaphylaxis, such as difficulty breathing, you should inject yourself in the outer thigh before seeking emergency medical help.
You May Like: Can You Drink On Allergy Meds
Can Immunocompromised People Receive The Covid
Yes. In fact, since people who are immunocompromised face an increased risk of severe disease if they get sick with COVID-19, they should do everything they can to protect themselves against the virus.
The main thing immunocompromised people should keep in mind regarding the vaccines is that the vaccines might not work as well for them. Since the vaccines rely on a strong immune system in order to work, a person who is immunocompromised might not get a strong effect from the COVID-19 vaccine. This means you could still be at risk of catching COVID-19, even after receiving the vaccine. We just dont know yet how well the vaccine works in people who are immunocompromised.
Guidelines For Administering The Vaccine
As mentioned before, only those with a known allergy to PEG or another vaccine ingredient should consider not getting vaccinated for COVID-19. And if you have an allergic reaction after the first shot, you shouldnt get the second shot.
If youve had a severe allergic reaction to another vaccine or injectable medication or have experienced anaphylaxis from any cause you can still receive the COVID-19 vaccine. However, your vaccination should be followed by a 30-minute observation period in a setting where personnel, equipment and supplies are present to manage anaphylaxis if needed.
Anaphylaxis commonly occurs within 30 minutes of exposure and would be unusual after 60 minutes, says Dr. Lang.
Patients with allergies to other medications, foods or inhalants can receive the COVID-19 vaccine with normal precautions. This typically includes a 15-minute observation period after the injection based on CDC guidelines
Again, if you have questions about COVID-19 vaccines or arent quite sure about what you should do, talk to your doctor.
Read Also: Do Twix Have Nuts In Them
Aafa: What Do We Know About The Clinical Trials For The Covid
Dr. David Stukus: We dont know specifically how many people had asthma or food allergies or allergic rhinitis. They didnt break it down by that when they reported this. There are other categories that are more important in the grand scheme of things to try to figure out whether the vaccine is safe and effective. But they werent excluded. The only potential allergy that was excluded specifically were those participants who may have had a severe allergic reaction to prior vaccines or any of the specific ingredients contained in this Pfizer vaccine.
Of note, the Pfizer vaccine does not contain any food proteins, food allergens, or food derivatives. It wasnt grown in embryos, so theres no egg or anything like that. We have to assume there were people with some of the more common chronic conditions, especially asthma. We have to assume there were people with asthma, allergic rhinitis, atopic dermatitis, and food allergies enrolled in these trials. Were not seeing any big scary signals from any group, let alone those.
Note: This is just an excerpt from the video. Watch the full video clip for the entire answer.

