Restrictions On Daily Activities
The risk of accidental exposure posed by PA extensively impacts daily activities, which may include playdates at friendsâ homes, attendance at daycare or afterschool care, parties and sports events, and camp and sleepovers.
4.2.1 Travel
Individuals with PA must take extra precautions in trip planning. A survey of this population in the UK highlighted several such considerations, including ability to understand the language at the destination, perceived experience on airlines, accessibility to medical care, familiarity with the destination and avoiding unfamiliar cuisines.
An international study of 3273 respondents with peanut and/or tree nut allergy from 11 countries found that 349 reactions to peanuts or tree nuts occurred aboard flights, with 13.3% of respondents receiving adrenaline for their reactions. In addition, flight crews were notified of the reactions in only 50.1% of cases. However, 69% of respondents made preflight accommodation requests .
4.2.2 School
Figure 4
Depending on the management strategies employed by children with PA and their families, the impact of PA on QoL is variable. Further, management of PA by paediatric allergy specialists has been shown to slightly improve QoL, demonstrating a crucial role for allergists and immunologists in helping allergic children and their families manage this burden.
New Research: Introduce Peanut Early For Peanut Allergy Prevention
In 2008, Dr. Gideon Lack and others observed that Israeli babies developed peanut allergies much less frequently than babies in the UK. In fact, the rate of peanut allergy prevalence in the UK was ten times greater than the peanut allergy prevalence in Israel. He noticed that Israeli babies started eating peanut in their first year of life, but the babies in the UK didnt eat peanut for several years. This prompted Dr. Lack to conduct further research on peanut introduction and peanut allergy prevention.
The landmark Learning Early About Peanut study, which Dr. Lack spearheaded, investigated whether consuming peanut early and often helped prevent children from developing a peanut allergy.
In the LEAP study , babies were divided into two groups. One group started to consume peanut three times per week starting at 4-11 months of age, and continued this regular peanut consumption until they reached 5 years of age. The other group avoided peanut completely until they reached 5 years of age.
The LEAP study found that introducing peanut to babies early and often reduced their peanut allergy risk by more than 80%.
- Early: Starting between 4 and 11 months of agethe earlier the better
- Often: 2-7 times a week for at least 6 months
In the LEAP study, only 3% of the children who ate peanut regularly developed a peanut allergy by age 5. But 17% of the children who avoided peanut developed a peanut allergy by the age of 5. Thats an 82.35% difference between the two groups.
The Extent Of This Issue
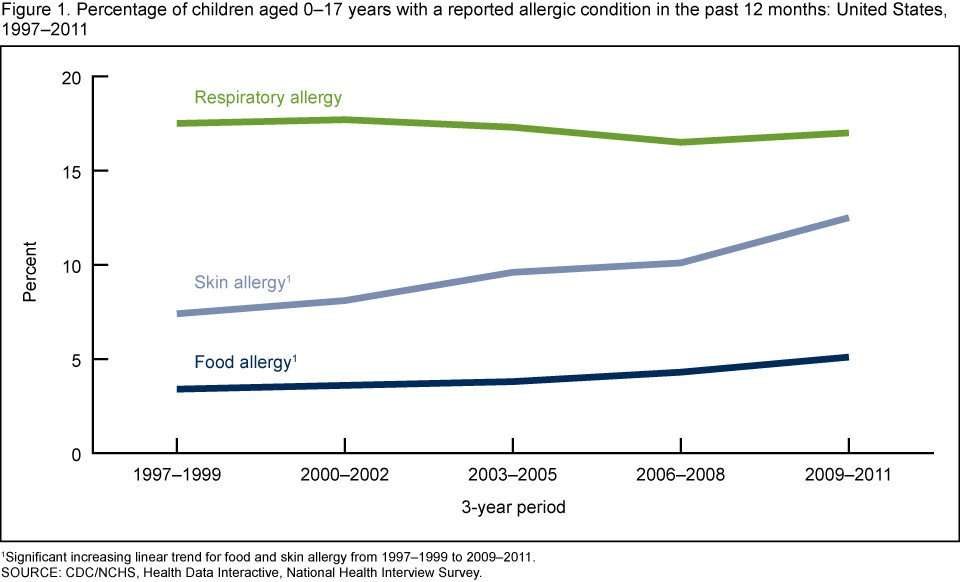
Many professionals believe allergies are increasing globally . Allergies, the most common chronic disease in Europe, affect more than 20% of the United Kingdom population . The Centres for Disease Control & Prevention reported from 1997-2008, peanut/tree nut allergies tripled in US children. In a US nationwide, cross-sectional telephone survey it was found the prevalence of peanut/tree nut allergy in children was 0.6% , 1.2% , 2.1% .
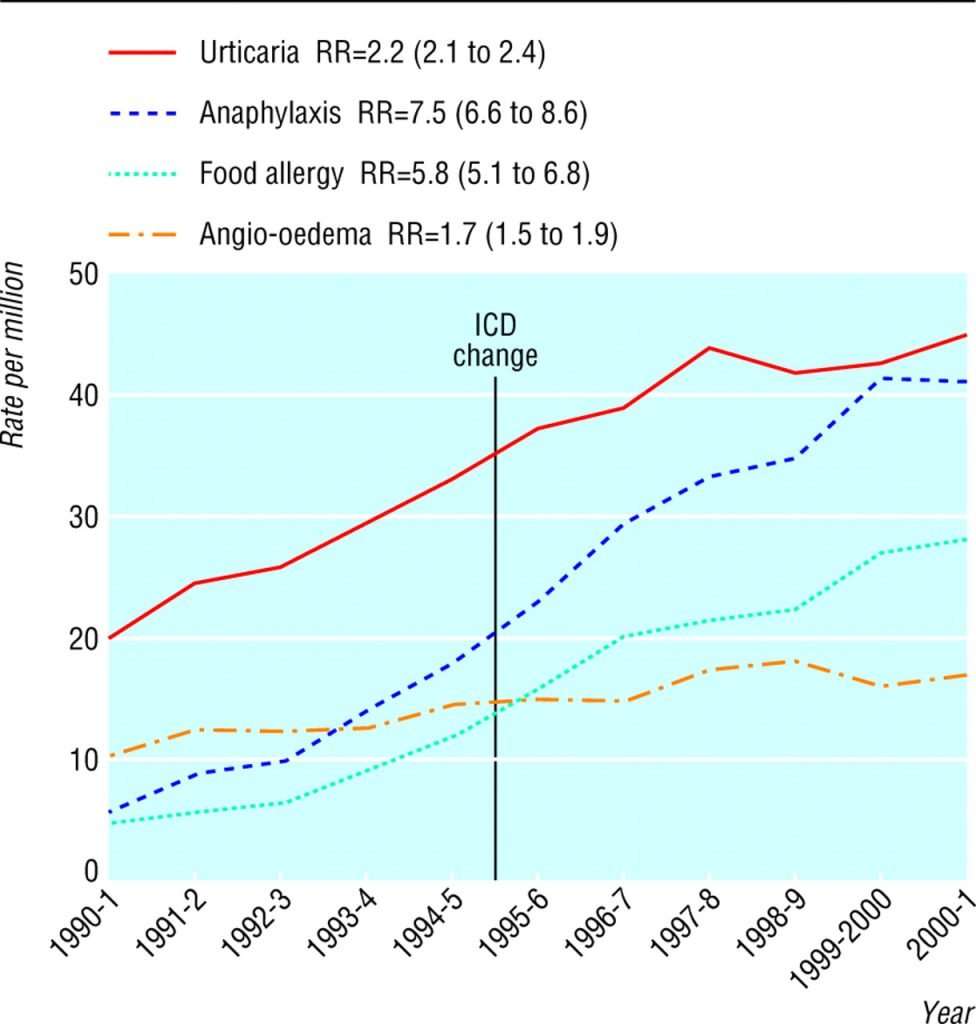
Hospital records provide strong evidence there was a 615% increase in the rate of hospital admissions in the UK for anaphylaxis from 1992-2012 , highlighting the rise of pressure on the NHS.
Allergies can cause disruption to daily tasks like sleeping, eating out and socialising . Studies show children with food allergies are more likely to be bullied , further leading to a negative impact on a childs emotional and physical health . Dr Rebecca Knibb, health psychologist, found having a food allergy causes greater distress and 40% of children and teens use avoidance strategies, avoiding events where food is present .
There is a large economic impact for those living with or caring for someone with a food allergy, especially without universal healthcare systems. It costs US families $25 billion annually , including medical costs, special food and absence from work . Consequently, there are adverse effects on the financial stability of families and the welfare of individuals.
Read Also: Intolerance Medical Definition
The Spinal Itch Pathway
After the pruriceptive primary afferent has been activated, the signal is transmitted from the skin into the spinal dorsal horn. In this area, a number of interneurons will either be inhibited or activated to promote activation of projection neurons, mediating the puriceptive signal to the brain. The GRP-GRPR interneuron system has been found to be important for mediating both histaminergic and non-histaminergic itch, where the GRP neurons activate GRPR neurons to promote itch
The Hygiene Hypothesis Or Microbial Hypothesis
This is currently the leading theory behind why food allergies are increasing. The idea is that an infants immune system needs to be exposed to germs to train itself to not overreact to things such as food, pollen or pollution. Children need to get dirty in order to build their immune systems. The environment impacts our micro-biome and those microbes interact with our immune system. In the increasingly sanitized world we currently live in, our immune systems are not educated at distinguishing between good and bad germs, leading to the increase in food allergies.
Recommended Reading: What Allergy Medicine Is Stronger Than Zyrtec
Does The Vitamin D Hypothesis Influence The Risk Of Food Allergy
Vitamin D, a vital nutrient for calcium absorption that aids the maintenance of healthy bones, plays a functional role in the immune system . It is absorbed through exposure to sunshine or consumed through supplements and food . Stored in the bodys fat cells, hydroxylation by the liver and kidneys forms calcitriol . The nutrients relation to food allergy, includes two contradicting arguments: vitamin D excess and vitamin D Deficiency hypothesis .
Vitamin D excess hypothesis claims that an increase in Vitamin D levels leads to increases in food allergies . Milner conducted a study showing children, who had vitamin D supplementation, were higher risk . On the other hand, a study by Kull et al found that regular fish consumption for the 1st year links to lower risks of sensitisation to foods by age 4 this may not be relevant in terms of effects of having nutrient excess.
The contradicting evidence leads to unsolved answers. However, when applying theories to real life the Vitamin D Deficiency hypothesis is stronger, due to the multitude of evidence and lifestyle changes in developed countries it is more likely populations have more time indoors. The above pro-con debate is further supported by the multitude of hypotheses discussed in this paper.
Molecular Diversity Of Itch Transmitting Primary Afferents
Using single-cell mRNA sequencing, sensory-modality specific primary afferent have been molecularly defined into clusters based on gene expression patterns. Here, 11 sub clusters were detected NF1-3, transmitting innocuous nociceptive information NF4-5, which transmit proprioceptive information NP1-3, transmitting itch information PEP1-2, nociceptive information and TH, which is involved in pleasant touch, The pruriceptive NP1-3 were shown to express genes related to histaminergic and non-histaminergic signaling, where NF1 expresses genes responding to lysophosphatidic acid , NP2 chloroquine-responsive genes , whereas NP3 expresses neuropeptides Nppb and Sst as well as genes involved in inflammatory itch . The histamine receptor gene Hrh1 was found in NP2 and NP3, suggesting that histaminergic itch is transmitted by both these pruriceptive sub clusters.
Recommended Reading: Can You Have Almond Extract With A Nut Allergy
The Risk Of Casual Contact
In those who are especially sensitive, reactions to peanuts can occur from ingesting just a trace amount. This can cause anxiety, especially for the parents of peanut-allergic children. However, research shows that touching, smelling, inhaling airborne particles or just being near peanuts is highly unlikely to cause a severe reaction : 180-2.)
Smelling the aroma of peanuts is not the same as inhaling airborne peanut particles that could potentially contain the allergenic protein. The aroma of peanuts comes from different compounds that cannot cause an allergic reaction. Also, highly refined peanut oil is not required to carry allergen labeling because the process used to purify the oil removes the protein, thereby making it no longer allergenic.
In one controlled study, 30 children with significant peanut allergy were exposed to peanut butter, which was either pressed on the skin for one minute, or the aroma was inhaled. Reddening or flaring of the skin occurred in about one-third of the children, but none of the children in the study experienced a systemic reaction.
What Causes A Peanut Allergy
Theres strong evidence that genetic factors may play a large role in the development of peanut allergies. A 2015 study of food allergies found that certain genes were present in 20 percent of the participants with peanut allergies.
Children are also being exposed to peanuts at an earlier age, which leads to increased allergic reactions. Other factors implicated in the rise of peanut-related allergic reactions include increasing environmental exposure. More people are adopting vegetarian diets and replacing meat with peanuts and tree nuts as a protein source. Food preparation methods may result in cross contamination or cross contact.
Also Check: What’s Better For Allergies Claritin Or Zyrtec
What Happened In The Past
The 1918 influenza pandemic was far the deadliest respiratory virus pandemic recorded in recent human history with over 50 million deaths worldwide. Although they used some of the same measures we are using now , the deaths slowed only after enough of the population had either acquired immunity through natural infection or died. Indeed, the first influenza vaccine was not developed until 1942, more than 20 years later. As judged by the amount of suffering and death from 1918 influenza , natural immunity is obviously a terrible way to get through a pandemic.
Similarly, measles was a highly transmissible respiratory virus that led to high levels of immunity among adults who were invariably exposed as children. However, measles led to deaths each year among the nonimmune until a vaccine was developed in 1963, largely restricting current measles outbreaks in the U.S. now to populations who decline to vaccinate. Smallpox also led to high levels of immunity through natural infection, which was often fatal. That’s why unleashing smallpox on a largely nonimmune population in the New World was so deadly. Only an effective vaccine and its administration worldwide, including among populations who declined smallpox vaccine at first via mandates could control and then eventually eradicate smallpox from Earth.
Fully vaccinated people are already now able to generate some antibodies against all the variants we know of to date, thanks to their bank of memory B cells.
Peanut Allergy Treatment Options
At Latitude Food Allergy Care, we provide oral immunotherapy to help patients improve their quality of life. OIT is approximately 85 percent effective for single or multiple food allergies and is safe for all ages.
The goal of oral immunotherapy is to continually expose the patient to increasing amounts of an allergen. As OIT progresses, the body is gradually desensitized and learns to adapt to the allergen. This allows for fewer dietary restrictions, and protects against severe or life-threatening reactions due to accidental exposure.
To determine whether a patient may be a candidate for OIT, our expert clinical team will evaluate existing conditions, collect full medical history, and discuss lifestyle. Latitude Food Allergy Care patients may also choose to include Palforzia in their treatment plan, an FDA-approved drug for peanut allergy treatment.
Recent research into peanut allergy treatment shows promising advancements for future therapies. New treatments may include sublingual immunotherapy , where small amounts of an allergen is held under the tongue for small periods of time, and epicutaneous immunotherapy , where an adhesive patch allows for minute amounts of an allergen to penetrate the skin.
Get started with a consultation to find out if Latitude is right for you
Don’t Miss: Zyrtec Generic Name
Peanut Allergy Rate Similar Across Globe
Researchers surveyed 5,300 households representing 13,534 people in 2008, a response rate of 42%.
The study is the first of its kind to incorporate all age groups within a national sample and to use the same methods over such an extended time period. It also is the first study in the U.S. to evaluate allergies to sesame seeds, according to the news release.
Tree nut allergies have increased from 0.2% in children in 1997 to 1.1% in 2008, the study says. Sesame allergy was reported in 0.1% of children and adults.
âOur research shows that more than 3 million Americans report peanut and or tree nut allergies, representing a significant health burden,â Sicherer says in the news release. âThe data also emphasize the importance of developing better prevention and treatment strategies.â
The American Academy of Pediatrics used to instruct parents to avoid peanut use until their kids reached age 3, but that has been rescinded, Sicherer says.
The researchers say the rate of peanut allergy they found in the U.S. is similar to results from studies using different methods in the United Kingdom, Canada, and Australia.
The study is published in the May 12 issue of the Journal of Allergy and Clinical Immunology.
Food Proteins In Vaccinations
There are others that suggest that food allergies are connected to the increase in vaccinations and the food proteins in the vaccines. There are studies that have demonstrated that food proteins that are in vaccinations induce food allergies. In the CDCc, Recommendation of the Advisory Committee on Immunization Practices it states that those with allergies to egg proteins should avoid certain vaccines. Some vaccines include gelatin like the MMR, Chicken Pox, Flu Shot and DTaP. Anyone that has experienced an allergic reaction after eating gelatin should avoid gelatin-containing vaccines. The same goes for the vaccines that include bakers yeast, eggs and peanut oil. The number of vaccines suggested we give our children has tripled since 1980 and so have food allergies.
Remember even if you do have food allergies you can still be healthy. It all goes back to building our immune systems to be as strong as possible. If you have had vaccines, antibiotics at a young age, you havent been eating healthy and you have been too clean, you can still make changes and support your health. Walk barefoot on the ground outside in the sun while eating an apple and drinking a kombucha. The dirt, the sun, the food and the probiotics can help build your immune system back up and heal.
Do you have food allergies?
I would love to hear how you live with them and why you might think that food allergies are increasing!
Be healthy!
Also Check: How To Read Allergy Test
Can Peanut Allergy Be Prevented
In 2017, the National Institute for Allergy and Infectious Disease issued new in order to define high, moderate and low-risk infants for developing peanut allergy. The guidelines also address how to proceed with introduction of peanut based on risk in order to prevent the development of peanut allergy.
The updated guidelines are a breakthrough for the prevention of peanut allergy. Peanut allergy has become much more common in recent years, and there is now a roadmap to prevent many new cases.
According to the new guidelines, an infant at high risk of developing peanut allergy is one with severe eczema and/or egg allergy. The guidelines recommend introduction of peanut-containing foods as early as 4-6 months for high-risk infants who have already started solid foods, after determining that it is safe to do so.
If your child is determined to be high risk, the guidelines recommend having them tested for peanut allergy. Your allergist may do this with a skin test or blood test. Depending on the results, they may recommend attempting to try peanut for the first time in the office. A positive test alone does not necessarily prove your child is allergic, and studies have shown infants who have a peanut sensitivity arent necessarily allergic.
Although parents want to do whats best for their children, determining what best means isnt always easy. So if your son or daughter is struggling with peanut allergies, take control of the situation and consult an allergist today.
Trying To Determine A Cause
One of the biggest challenges with peanut allergies in both children and adults is that it’s difficult to predict who will develop an allergy, especially because some children outgrow the allergy, while others will have it for life. Also, adults who may have been able to eat peanut butter every day for decades can suddenly have an allergic reaction.
Prediction is nearly impossible, in large part because no one knows exactly why peanuts are so problematic, which makes it difficult to understand why prevalence is rising so quickly, says Schuval. There are several theories, though, and many experts believe multiple factors are involved.
For example, Schuval says changes in agricultural practices may play a role, or higher rates of inflammation from eating a Western-style diet that’s high in sugar and saturated fat. Another key idea is the “hygiene hypothesis,” says Jeffrey Neal, MD, an otolaryngologist at Abingdon Ear, Nose & Throat Associates in Virginia.
“There’s an idea that we now have less exposure to viruses and bacterial infection throughout our lives,” he says. “Essentially, because we live in more sterile environments with air conditioning and that we’re not outside as much, this leaves our immune system unbalanced and predisposes us to allergic reaction. This is true for both adults and children.”
Despite the uncertainty around potential causes, there are two factors that make kids at higher risk, Schuval says:
You May Like: What Allergy Medicine Is Stronger Than Zyrtec
Is It True That Some Allergists Have People Consume Small Amounts Of Foods Theyre Allergic To In Order To Build Up Tolerance
Dr. Taylor:
I would suggest that people talk to their allergists before they try that. The allergist may, in some cases, suggest periodically trying the food to see if youve outgrown your allergy, but you should do that only with expert advice. It can be a risky proposition as it is really hard to control the dose. It has to be done under expert medical guidance doing it at home is not recommended.
If you are experiencing problems you think are associated with food allergies, please visit your physician or allergist.

