Can An Infant Outgrow Cows Milk Allergy
Most children will outgrow cowsâ milk allergy.
Studies show that most children with non-IgE-mediated reactions will outgrow cowsâ milk allergy by the time they are 3 years old.
For children with IgE-mediated reactions, studies show that about half of these children will outgrow cowsâ milk allergy by the time they are 5 years old. Evidence suggests that a cows’ milk protein allergy is more likely to persist in these children if they have asthma or allergic rhinitis, or if they have more severe reactions or higher milk-specific IgE antibody levels. Even so, itâs rare for adults to have a cowsâ milk allergy.
Dietary Restrictions For Cows Milk Allergy Should Be Supervised
Exclusion and reintroduction of cow’s milk and other dairy foods should only be undertaken with advice from a medical specialist , particularly in cases of anaphylaxis. If long-term exclusion is required, an alternative source of calcium and protein is needed, to ensure adequate nutrition and growth.
Excluding foods from the diet during breastfeeding is rarely required, and if recommended, the maternal nutritional intake should be supervised, assessed and reviewed by a dietitian. Assessment and review by a dietitian is also recommended for babies and children who need to exclude cows milk and other dairy foods.
Diagnostic Tests For Milk Allergy
Your doctor may require a physical test and a history of your symptoms for diagnostic purposes. Make sure you mention all dairy foods youve been eating especially before symptoms occur. Be sure to mention these types of food as they can help narrow down the diagnosis:
- Yogurt, milkshakes, malts
- Chocolates and caramels
- Butter and margarine
A history of symptoms and physical tests may be insufficient in diagnosing allergies. As such, you may be asked to take diagnostic tests to pinpoint the exact cause of your symptoms.
Doctors may use blood tests to diagnose allergies. People with more than 200 KU/L of IgE in their blood may be at greater risk of allergic reactions.
A skin test is also a useful diagnostic method. Your doctor will expose a portion of your skin with milk protein and see how your body reacts. The presence of hives or rashes indicates an allergic reaction to either whey or casein protein.
You may also need to take an oral challenge, in which you will consume different types of foods with varying milk content under the supervision of your doctor. Your doctor will slowly increase your intake of certain foods and then observe whether you react to those with milk.
Recommended Reading: Is Imitation Almond Extract Safe For Nut Allergies
Milk Allergy Vs Milk Intolerance
Milk allergy and milk intolerance differ when it comes to the affected organ systems. Milk intolerance, also known as lactose intolerance, is an issue of the digestive system. Milk allergy is an immune system condition.
Another difference between milk allergy and milk intolerance is the active agent causing your symptoms. Casein and whey, the two dominant proteins in milk, cause milk allergies. Casein is the protein in solid milk curd, while whey is the remnant liquid. The inability to digest lactose because your body does not produce lactase causes lactose intolerance.
Despite these differences, milk allergy and milk intolerance are often confused with each other. This phenomenon may likely be because of its similarities in symptoms.
Similar symptoms include an upset stomach and diarrhea. However, a milk allergy also has other symptoms such as:
- Wheezing and coughing
- Swelling lips, tongue, or throat
- Itchy mouth, tongue, or throat
Should you notice someone with these symptoms, rush them to the ER for an epinephrine shot. As it is such a life-threatening situation, properly diagnosing milk allergy is necessary. Diagnosis is essential, so you experience the least complications and symptoms possible.
Points De Repre Du Rdacteur
- Lallergie aux protéines du lait peur survenir durant lallaitement au biberon ou durant lallaitement maternel, habituellement avant lâge dun an. Les manifestations initiales peuvent être cutanées , mais elles peuvent aussi être dordre respiratoire, digestif ou nutritionnel. Certains nourrissons présentent dabord des pleurs irréductibles et refusent toute nourriture.
- Lhistorique permet de soupçonner une allergie aux protéines du lait. Les investigations possibles incluent la provocation alimentaire, le prick-test, la mesure du taux sérique des anticorps IgE spécifiques et lépidermoréaction.
- Le traitement cherchera principalement àéviter lallergène tout en maintenant un régime nourrissant et équilibré, pour le nourrisson comme pour la mère lallaitement au sein peut être poursuivi si la mère évite les allergènes. Le poids du bébé doit être étroitement surveillé.
- Lallergie aux protéines du lait peut être traitée avec succès en soins primaires avec le soutien dune diététicienne les autres spécialistes ne devraient être consultés quen cas dallergie sévère ou déchec du traitement standard et quand des tests dallergie spécifiques sont indiqués.
Recommended Reading: What’s The Best Children’s Allergy Medicine
Avoiding A Milk Allergy Reaction
If You’re Breastfeeding
If your breastfed infant has a milk allergy, talk to the allergist before changing your diet.
If You’re Formula Feeding
If you’re formula feeding, your doctor may advise you to switch to an extensively hydrolyzed formula or an amino acid-based formula in which the proteins are broken down into particles so that the formula is less likely to trigger an allergic reaction.
You also might see “partially hydrolyzed” formulas, but these aren’t truly hypoallergenic and can lead to a significant allergic reaction.
If you’re concerned about a milk allergy, it’s always best to talk with your child’s doctor and work together to choose a formula that’s safe for your baby.
Do not try to make your own formula. Commercial formulas are approved by the U.S. Food and Drug Administration and created through a very specialized process that cannot be duplicated at home. Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
If you have any questions or concerns, talk with your child’s doctor.
What Should I Do If I Think My Baby Is Allergic Or Intolerant To Cows’ Milk
If you think your baby is having a reaction to cows’ milk, see your GP to discuss your concerns.
They will be able to assess if your baby’s symptoms may be caused by a cows’ milk allergy or something else. Make sure you get medical advice before taking cows’ milk out of your child’s diet as it contains important nutrients.
Read Also: Can Allergies Give You A Headache
Causes Of Milk Allergy In Infants
Although it is very hard to predict what is about to happen in future, it is quite sensible to take precaution and to identify the causes of milk allergy in infants. It has been seen that infants whose families hold an allergic history have a higher probability of developing allergies among infants as well. Yet some studies have conjointly shown that environment plays a huge role in developing hypersensitivity reaction in infants. All food allergies result when immune system does not react appropriately. The Immune system is capable enough to identify milk products which are harmful. So once it detects some harmful protein, it permits the production of Immunoglobulin to counterbalance the Protein .
Generally there are two varieties of protein found in cows milk that can cause an allergic reaction. One of them is Casein that is found in solid part of milk and Whey in liquid part of milk that remains when milk curdles. Your Infants might be allergic to both protein and they are difficult to avoid due to their presence in majority of baby food available in the markets. It has been observed that people who react and shows allergies to cows milk also have high possibility to react to buffalo, goat and sheeps milk as well.
Algorithm For The Diagnosis And Management Of Cmpa In Exclusively Breast
Breast feeding is the gold standard for milk feeding in infant nutrition and is recommended exclusively for the first 4 months of life at least. The incidence of CMPA is lower in exclusively breast-fed infants compared to formula-fed or mixed-fed infants. Indeed, only about 0.5% of exclusively breast-fed infants show reproducible clinical reactions to CMP and most of these are mild to moderate. This might be related to the fact that the level of CMP present in breast milk is 100000 times lower than that in cows milk. In addition, immunomodulators present in breast milk and differences in the gut flora in breast-fed and formula-fed infants may contribute to the prevalence of CMPA in breast-fed compared to formula-fed infants. The most frequent symptoms of CMPA in exclusively breast-fed babies are listed in and include general dermatological and gastrointestinal manifestations.
The elimination diet should be continued for a minimum of at least 2 weeks, and up to 4 weeks in cases of atopic dermatitis or allergic colitis. The mother will require calcium supplements during the elimination diet. If the elimination diet fails to improve the symptoms, the mother should resume her normal diet and a referral to a specialist should be considered, depending on the type and severity of the infants symptoms.
Also Check: What Age Do Pollen Allergies Start
Risk Factors For Milk Allergy In Infants
There are various risk factors which may lead to developing of milk allergy among Infants. These factors are:
- Age: Studies have shown that 2 to 7.5 percent of infants under the age group of 1 are allergic to cows milk. But as they grow, their immune system develops and their allergy towards cows milk also vanishes.
- Family History: Babies are more prone to food allergy if one of their parents holds an allergic history or any type of allergy. It can be asthma, fever, eczema or hives.
- Other Possible Allergies: Lots of children are allergic to food and other things. Milk allergy is the first kind of allergy seen in infants. Food allergy can also lead to atopic dermatitis which is a chronic infection of the skin which occurs due to food allergy.
The Role Of In Vitro And In Vivo Testing For Cmpa
None of the available diagnostic tests prove or disprove that the child suffers from CMPA. Because of these limitations, allergen elimination diets and challenge procedures remain the gold standard for the diagnosis of mild-to-moderate CMPA in formula-fed infants. Clinicians can consider performing SPT or determining specific IgE against whole milk or single individual CMPs. SPTs with fresh cows milk resulted in larger wheal diameters than with commercial extracts, although the difference was not significant. Conversely, wheal diameters were significantly larger with fresh foods for the other food allergens. The overall concordance between a positive prick test and positive challenge was 58.8% with commercial extracts and 91.7% with fresh foods. These results indicate that fresh foods may be more effective for detecting sensitivity to food allergens. Fresh foods should be used for primary testing for egg, peanut and cows milk sensitivity.
Patch testing in the investigation of CMPA is still a subject of on-going research and can aid the diagnosis of non-IgE-associated reactions. Patch tests may contribute to the diagnosis of food allergy, even when SPT and RAST were negative. However, the patch test method needs to be standardised.
Don’t Miss: What Piercing Helps With Allergies
Milk Intolerance In Babies And Children
6-minute read
Some babies and children have a reaction when they drink cow’s milk or formula made from cow’s milk. This could be due to 2 things: a lactose intolerance or an allergy to milk. If your child has one of these conditions, you will have to alter their diet to cut down on milk or avoid it altogether.
- wheezing or difficulty breathing
- they are pale and floppy or unconscious
Treatment For Milk Allergy In Infants
If your infant is prone to milk allergy or you are breastfeeding, then it is very significant to limit the intake of milk or dairy products as the milk protein, which causes allergy can get into your breast milk while feeding and it may affect your infant health. To treat this problem, you should contact your doctor or consult a dietitian regarding finding alternative and best sources of vital nutrients and to consume as an alternative to milk products which may cause allergy to your infant.
Since 2006 a resolution has been passed to all food makers, stating that it has been vital to clearly mention the ingredients used in packaged baby food which will surely be helpful to mothers in choosing the right baby food.
If you are feeding packed baby food, then your doctor might tell you to use soy protein based baby foods. In some cases, infant cannot stand soy, then the one and last option left with doctor is that he/she may suggest you to choose a hypoallergenic formula that has the essential proteins broken into smaller particles and the food is less allergic and will not cause any allergic reaction to infant.
Don’t Miss: What To Drink For Allergies
Delayed Reactions To Cows Milk And Other Dairy Foods
Delayed reactions usually occur after two or more hours after consuming cows milk or other dairy foods. Symptoms may include an increase in eczema or delayed vomiting and/or diarrhoea. Allergy tests to cows milk are usually negative for these reactions.
Diagnosis should be made in consultation with a specialist paediatrician and/or clinical immunology/allergy specialist. This usually involves excluding cows milk and other dairy foods from the diet for a trial period of one to four weeks to check for a clear improvement. A planned reintroduction of cows milk and other dairy foods should occur to confirm diagnosis before longer term exclusion is advised.
What Are The Symptoms
Symptoms of a milk protein allergy often take place within minutes to a few days of exposure to cows milk. Infants may be exposed through formula or the breast milk of mothers who ingest cows milk or products made from cows milk.
Allergy symptoms may be gradual or occur rapidly.
Symptoms with a gradual onset may include:
- loose stools, which may be bloody
No single test exists to diagnose a milk protein allergy. Diagnosis occurs after reviewing symptoms and going through a process of elimination to rule out other medical conditions. Tests may include:
- allergy tests, including skin prick or patch tests
Your healthcare provider may recommend an elimination diet.
They may have you feed your baby formula thats free from cows milk or ask you avoid cows milk if youre breastfeeding.
Proteins from the foods a breastfeeding mother eats can appear in breast milk within 3 to 6 hours and can remain for up to 2 weeks. Typically, an elimination diet will last for at least 1 to 2 weeks. Cows milk is then reintroduced to see if allergy symptoms return.
Breast milk is nutritionally balanced, offers protection against illnesses and infections, and reduces the risk for Sudden Infant Death Syndrome . Babies who are breastfed are less likely to develop food allergies and even chronic diseases later in life.
If youre breastfeeding and your child develops a cows milk allergy, youll need to make dietary changes. Eliminate dairy products, including:
- processed and packaged foods
Read Also: How To Help A Sore Throat From Allergies
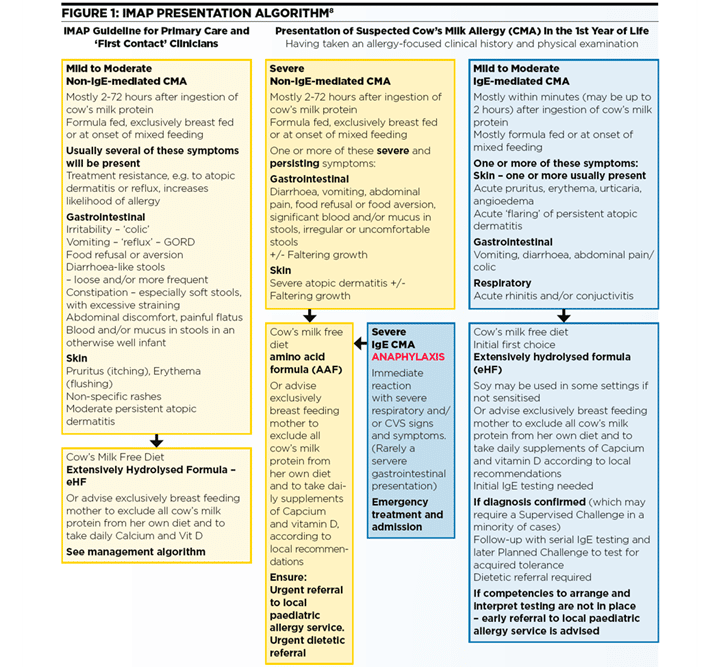
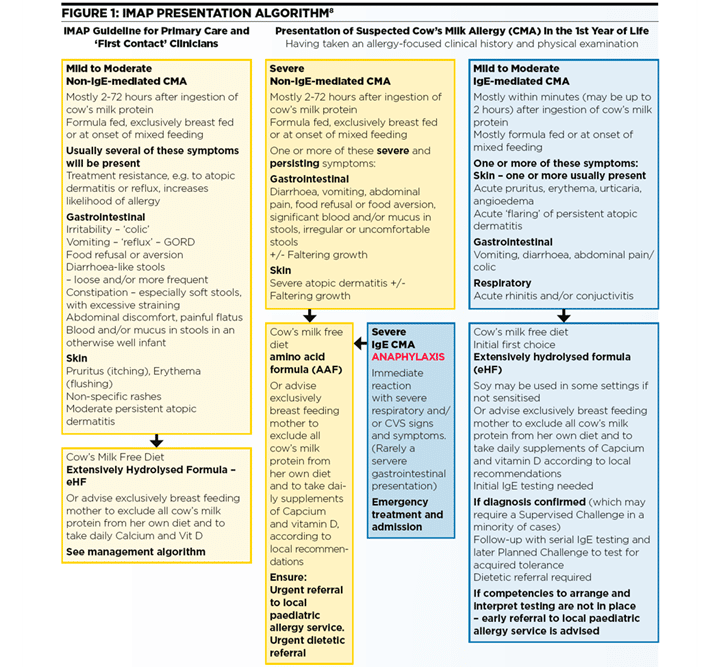
A Child Fed With Cow’s Milk Formula With Mild
Figure 2
In infants with immediate symptoms or late symptoms , constipation) a CMPA can be suspected . Other causes are to be considered for patients unresponsive to treatment. Infant colic is not unanimously considered as a consequence of CMPA. The paediatrician has to consider the opportunity of a cow’s milk free diet in the most troublesome cases . Mild immediate reactions may be of difficult interpretation because they can be the result of causes different from CMPA. However, if these symptoms are strongly related to cow’s milk ingestion, we recommend to eliminate cow’s milk and follow the algorithm for severe reactions .
Regarding delayed onset gastrointestinal symptoms, other pathologies should be excluded before investigating allergic sensitization.
In mild atopic dermatitis, investigations for CMPA are not necessary in the absence of a clear relation between cow’s milk intake and onset of symptoms.
When a CMPA is suspected, infants should go on a 2-4 week diet without cow’s milk protein. Four weeks should be considered for chronic gastrointestinal symptoms. Infants should be fed with eHF or SF in children aged more than 6 months and without gastrointestinal symptoms.
When there is strong suspicion of IgE-mediated reactions, in infants who do not respond to a diet with eHF or SF an attempt may be made with a 14-days diet with AAF.
Symptoms Of Cows’ Milk Allergy
Cows’ milk allergy can cause a wide range of symptoms, including:
- skin reactions such as a red itchy rash or swelling of the lips, face and around the eyes
- digestive problems such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction, or anaphylaxis, is a medical emergency call 999 or go immediately to your local hospital A& E department.
Recommended Reading: Does Quercetin Help With Allergies
What Are The Symptoms Of Cows Milk Allergy
A wide range of symptoms can be triggered by a cows’ milk protein allergy, usually involving the skin, gastrointestinal tract, and respiratory tract. Those that involve the respiratory tract often appear along with other symptoms. These include:
IgE-mediated symptoms
- Skin reactions: Itchiness, reddening of the skin, sudden itchy rash , or swelling, most often of the lips, face, and around the eyes
- Gastrointestinal reactions: Swelling of the lips, tongue, or palate in the mouth, itchiness in the mouth, nausea, vomiting, colicky abdominal pain, or diarrhea
- Respiratory reactions: Itchy nose, sneezing, runny nose, congestion, cough, wheezing, or shortness of breath
Non-IgE-mediated symptoms
- Skin reactions: Itchiness, reddening of the skin, or eczema
- Gastrointestinal reactions: Acid reflux or gastro-esophageal reflux disease , loose or frequent stools , blood or mucus in poo, abdominal pain, colic, constipation, refusing food or aversion to food, redness in the perianal area, tiredness
- Respiratory reactions: Cough, wheezing, or shortness of breath
In rare cases, a child may have an anaphylactic reaction, which requires emergency medical help because it can be fatal. Call an ambulance if you think your infant is struggling to breathe or is floppy.
A cows’ milk protein allergy can sometimes lead to complications due to malabsorption or poor nutritional intake. The child may get chronic iron deficiency anemia or fail to thrive.

